Rakesh Patel, MD, Medical Director of the Targeted Radiation Institute at Western Radiation Oncology, Pleasanton, California, was the invited discussant of the second study. He noted that in spite of well documented equivalent survival rates between the surgical approaches, mastectomy rates are increasing across all ages.
Rakesh Patel, MD, Medical Director of the Targeted Radiation Institute at Western Radiation Oncology, Pleasanton, California, was the invited discussant of the second study. He noted that in spite of well documented equivalent survival rates between the surgical approaches, mastectomy rates are increasing across all ages.
“There are multifactorial reasons for this,” he pointed out, “including improved reconstruction options, use of preoperative MRI, identification of high-risk patients with genetic predispositions, and concerns about long-term radiotherapy impact. And all the factors have a greater influence in younger patients.”
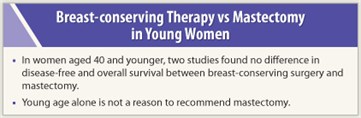
Mastectomy does prevent more locoregional recurrences, he acknowledged, and it is believed that “for every four local recurrences prevented, one life is saved.” But this is only true when the reduction in local recurrence is substantial, which is generally not the case for node-negative early breast cancer in young women.
Complex Decision
 The choice between breast-conserving therapy and mastectomy can be complex, he emphasized, and should take into account biologic factors, genetic risk, the variable effectiveness of systemic therapy, the need for radiation therapy postmastectomy, the potential for long-term side effects, and quality of life.
The choice between breast-conserving therapy and mastectomy can be complex, he emphasized, and should take into account biologic factors, genetic risk, the variable effectiveness of systemic therapy, the need for radiation therapy postmastectomy, the potential for long-term side effects, and quality of life.
Commenting during the press conference, Andrew D. Seidman, MD, of Memorial Sloan-Kettering Cancer Center, agreed. “We are starting to look beyond the usual prognostic factors such as tumor size, grade, and lymph node, estrogen receptor, and HER2 status, and are moving into biologic subtyping to obtain additional information regarding the risk of relapse.” He said he considers many factors when recommending a surgical approach. One reason mastectomy has become more palatable, he added, is the recognition that young women are immediately referred for a breast reconstruction consultation. ■
Disclosure: Drs. Patel and Seidman reported no potential conflicts of interest.