In the 50 years now since my fellowship training, there have been major advances in the diagnosis, staging, prognostic scoring, treatment, and response assessment of lymphomas. To conjure up the future, we must first appreciate the present by understanding how it arose from the past.1 So, a trip in Mr. Peabody’s Wayback Machine would be very instructive.
Classification of Lymphoma
Diagnosis would not have been possible without Antonie von Leeuenhoek, who was in the fabric industry and needed a better way to evaluate his materials. So, in about 1668, he invented the microscope. Fast forward about 300 years when Karl Lennert identified centrocytes and centroblasts in lymph nodes, paving the way for a series of classifications of lymphomas through the Rappaport, Berard, Working Formulation, Lukes-Collins (REAL) and finally three iterations of the World Health Organization (WHO) blue book. This world order unfortunately collapsed around 3 years ago, with a schism between the WHO (HAEM-5) and the International Consensus Conference. The word is that there will be a unified classification next year.
Lesson 1: There are 3 things certain in life: (1) You will pay taxes; (2) You will die; (3) There will be a new lymphoma classification.
Lymphoma Staging
In 1950, Vera Peters, a Canadian radiation therapist given credit for being the first to appreciate the curability of Hodgkin lymphoma with radiation, published the first widely recognized, albeit rudimentary, three-stage system. This system was followed in 1968 by the Rye classification and eventually, in 1971, by the durable Ann Arbor classification (modified by the Lugano Classification of 2014).2 For decades, staging essentially involved torture of the patient with laparotomy and splenectomy; bone marrow trephine biopsy; and the lymphangiogram, in which a needle was inserted between the patients’ toes and a permanent blue dye injected, so node size could be followed with radiographs.
Current anatomic systems have been relatively unchanged for 75 years, despite a conversion to systemic treatment, and they do not adequately direct therapy.— BRUCE D. CHESON, MD, FACP, FAAAS, FASCO
Tweet this quote
Lesson 2: The initial rationale for staging was to provide anatomic guidance for the radiation therapist. Current anatomic systems have been relatively unchanged for 75 years, despite a conversion to systemic treatment, and they do not adequately direct therapy.
Prognostic Scoring Systems
The intent of prognostic scoring systems has been to guide treatment and allow for comparisons among studies. Large B-cell lymphoma started with the International Prognostic Index (IPI) followed by a string of derivatives—age-adjusted IPI, rituximab IPI, NCCN-IPI, and others. For follicular lymphoma, there was the FLIPI score (prior to the era of rituximab), the FLIPI-2 (in the rituximab era), and the short-lived M-7 FLIPI. The Mantle Cell International Prognostic Index requires a calculator, and the Hodgkin International Prognostic Index really does not identify a particularly poor-risk population.
Lesson 3: Current prognostic scores are decades old and do not reflect tumor biology. They do not direct therapy and are not clearly relevant using current treatments. Moreover, prognostic factors change with more effective treatments.
Evolving Treatment of Lymphoma
The treatment of lymphoma initially evolved very slowly. For example, CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) came about in 1979, when the Southwest Oncology Group demonstrated its superiority over COP. However, the study was conducted in patients with “diffuse” lymphomas, likely a mix of B-cell, T-cell, large B-cell, mantle cell, and whatever else. Nevertheless, it became the standard.
Being chained to R-CHOP and bendamustine/rituximab is counterproductive to progress and impedes the road to a chemo-free world.— BRUCE D. CHESON, MD, FACP, FAAAS, FASCO
Tweet this quote
“The definition of insanity is doing the same thing over and over again and expecting different results” (attributed to Albert Einstein, although probably not said by him.) Over the ensuing years, CHOP was challenged by numerous second-generation chemo combinations from various groups and centers, all looking more promising in phase II studies. However, they failed the phase III comparison of the SWOG-led High Priority study.3 Nonetheless, the parade of CHOP modification continued, with no effect, until Coiffier et al demonstrated that the addition of the targeted agent rituximab, not chemo, improved outcomes. In the accompanying editorial, I suggested that future progress would require the addition of additional targeted agents, not chemo. But this pattern was not limited to R-CHOP.
Twenty-five years ago, I brought bendamustine into the United States, and we conducted the first three trials, which led to its approval by the U.S. Food and Drug Administration in relapsed and refractory indolent lymphoma. The German StiL Group showed that bendamustine-rituximab was superior to R-CHOP in indolent and mantle cell lymphomas. But, true to form, various chemo agents were added to bendamustine, with no benefit.
Lesson 4: Shuffling chemo drugs, doses, and schedules has been a bust. Being chained to R-CHOP and bendamustine/rituximab is counterproductive to progress and impedes the road to a chemo-free world.
Response Criteria for Lymphomas
Much of my career has focused on designing response criteria for acute myeloid leukemia, myelodysplastic syndromes, chronic lymphocytic leukemia, and notably non-Hodgkin lymphoma (NHL) and Hodgkin lymphoma (HL). Prior to 1999, the different groups and centers varied in how and when response was assessed and with what procedures (eg, laparotomy, lymphangiogram, gallium or CT scan), what size node should be considered normal, and how much enlargement should be considered progressive disease.
Although there was great variability in how complete remission was defined, there was unity in defining a partial response as at least a 50% reduction in tumor size. That value was determined very scientifically. Charles Moertel of the Mayo Clinic conducted what I call the Princess and the Pea experiment, named after the Hans Christian Andersen fairy tale. He brought together 16 expert oncologists who measured 12 simulated tumor masses placed under a mattress. Of them, two pairs were identical in size. Only with a difference of at least 50% could the size of the masses be differentiated. Thus, there is no biological justification for the cutoff values for partial remission or progressive disease.
To reduce all the discrepancies, in 1999, I convened a group of lymphoma experts to draft the first widely adopted CT-based response criteria for NHL, subsequently adopted for HL as well. The world changed, however, with the availability of the PET scan, which was more sensitive and specific than the CT scan. In a group of patients with large B-cell lymphoma (LBCL), we demonstrated that PET could distinguish fibrosis or sclerosis from viable tumor.
Such observations led to a revision of the response criteria in 2007, primarily for diffuse LBCL (DLBCL) and HL, because that is where there were the majority of PET data. The criteria were a bit more complicated, because they distinguished between fluorodeoxyglucose (FDG)-avid and non–FDG-avid lymphomas. The general availability of that technology led to its overuse, which I referred to as “Heavy PETting,” and was shown to provide no advantage to scanning on the basis of clinical judgment and laboratory data.
Publication of the 2007 recommendations was followed by at least two pivotal events: the development by Michel Meignan and colleagues of the semiquantitative Deauville 5-point scale for measuring PET response4 and the demonstration that PET was useful in other histologies as well, such as follicular lymphoma. Numerous meetings subsequently led to what is now considered the bible of staging and response: the Lugano Classification.2 The assessment criteria were voluminous and cumbersome, but they have stood fast for over a decade. One of the positive features was based on reports from several groups that PET/CT was better at detecting bone marrow involvement in DLBCL and HL, and the trephine was no longer needed in most patients. A subsequent CALGB study confirmed its limited usefulness in follicular lymphoma as well.
Although total metabolic tumor volume and radiomics have been used to develop new prognostic strategies, it is ctDNA that has the greater potential to advance the prognostic and therapeutic field.— BRUCE D. CHESON, MD, FACP, FAAAS, FASCO
Tweet this quote
However, numerous issues arose, suggesting that a different approach might be needed. For example, the Deauville scale included vague terms such as “moderately” and “markedly,” which were inadequately quantitative and lacked a threshold for patient response and progressive disease, and the Deauville score 4 did not always correlate with actual patient response.
Moreover, several studies of time-dependent outcomes in follicular lymphoma failed to show a correlation with similar response rates. This observation was attributed to the fact that measurable residual disease (MRD) was a more sensitive predictor of outcome.
Another problem came with the introduction of immunotherapies; they were sometimes associated with flare reactions, which could be confused with progressive disease. Thus, we developed the LYRIC criteria to help distinguish between the two.
Lesson 5: PET interpretation remains too arbitrary and vague. It is inadequately sensitive and not clearly correlating with outcome: patients with PET-negative disease still recur, whereas some patients with PET-positive disease do not. Of note, the addition of a biomarker, such as MRD or circulating tumor DNA (ctDNA),5 would improve response assessment.
Roadmaps to Change
As a result, a workshop was organized for the 17th International Conference on Malignant Lymphoma (ICML) in Lugano, Switzerland, in June 2023. The major question was whether a revision of the Lugano Classification was warranted: should there be a change from anatomic to prognostic staging; clarification of the role of PET/CT; and how to incorporate new technologies, including total metabolic tumor volume6 and ctDNA.5 The conclusion was that, indeed, a modification was warranted, but there was little agreement on how to do it. The ICML was charged with bringing together a next generation of scientists to move the direction forward.
We already have several roadmaps on how to get there. One of the first observations that stimulated a consideration of patient-directed treatment was the recognition over 2 decades ago that LBCL was represented by two cells of origin: the activated B-cell (ABC) and the germinal center B-cell (GCB). However, although the two had different outcomes, the recent POLARIX trial was the first to demonstrate its therapeutic significance. Whereas the regimen of polatuzumab vedotin plus rituximab, cyclophosphamide, doxorubicin, and prednisone achieved a modest advantage over R-CHOP in progression-free survival, it was only effective in the ABC group. Diving deeper into the genetic profile, we found it was only in those patients with the so-called Cluster 5 subtype.
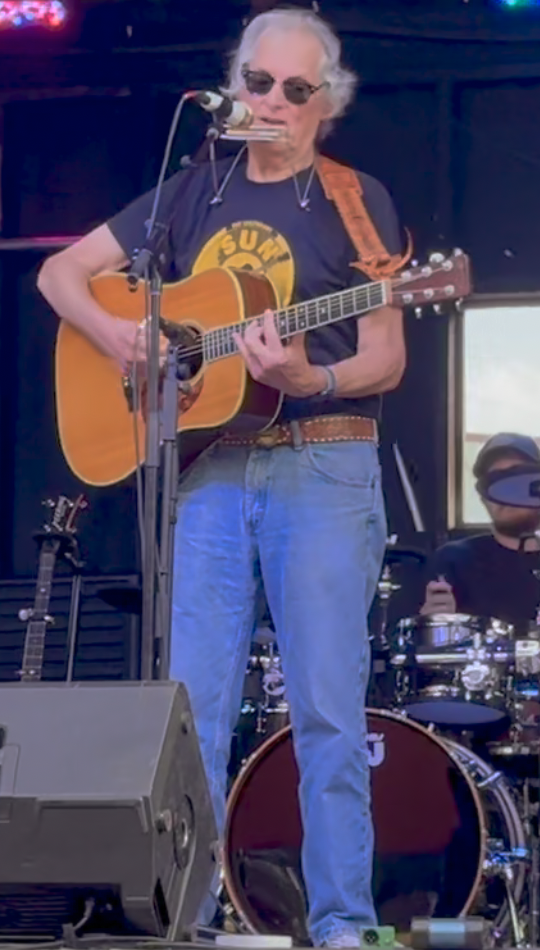
50+ years later and still rockin’: Dr. Cheson has been a researcher and clinician for the past 50+ years. He is also a country rock guitarist and has played with numerous groups such as the Oncotones at ASCO, with Kimberley Dahme (of the group Boston), and country stars Martin and Kelly at the Harmony 4 Hope music festivals supporting the Lymphoma Research Foundation, and other oncology meetings globally.
The newly considered entity of Dark Zone lymphomas includes those with a molecular Burkitt or double-hit signature, with important therapeutic implications. One example of the importance of this observation is that these patients fare poorly with chimeric antigen receptor (CAR) T-cell therapy and should probably be considered for other options. Similarly, when we look at microenvironmental signatures, only those patients with LBCL who have a “normal” archetype showed benefit from CAR T-cell therapy, unlike those with a so-called hot or cold signature. These observations and others beg the patently rhetorical question of whether we should continue with CHOP- or bendamustine-based therapy in a one-size-fits-all approach or instead design approaches based on tumor biology.
Although total metabolic tumor volume and radiomics have been used to develop new prognostic strategies, it is ctDNA that has the greater potential to advance the prognostic and therapeutic field. Indeed, I have suggested a two-stage, disease-specific system based on total metabolic tumor volume, ctDNA and biological prognostic factors to replace the traditional four-stage anatomic system. Similarly, I have proposed a more clinically relevant set of response criteria based on total metabolic tumor volume and ctDNA. Many centers globally do not yet have access to this technology, but it will be coming soon. After all, we developed the 2007 response criteria in a setting where PET/CT was still considered a new-fangled contraption in parts of the world. Whether my criteria will be met with favor by the new ICML working group remains to be seen.
Final Lesson: To improve patient outcomes, a revolution is clearly needed for integrating staging, prognosis, treatment, and response assessment in the context of the remarkable proliferation of exciting new, nonchemo therapeutic agents for lymphoma.
DISCLOSURE: Dr. Cheson has served as a consultant or advisor to AbbVie, MorphoSys, Karyopharm, Kite, Epizyme, Roche-Genentech, Janssen, Pharmacyclics, AstraZeneca, BeOne Medicines (formerly BeiGene), and Bristol Myers Squibb; and his institution has received research funding from AbbVie, Roche-Genentech, Trillium, and AstraZeneca.
REFERENCES
- Cheson BD: Equal parts dreams, luck, and madness: Conjuring a new future for lymphoma therapy. 2025 International Conference on Malignant Lymphoma. Presented June 18, 2025.
- Cheson BD, Fisher RI, Barrington SF, et al: Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: The Lugano classification. J Clin Oncol 32:3059-3068, 2014.
- Fisher RI, Gaynor ER, Dahlberg S, et al: Comparison of a standard regimen (CHOP) with three intensive chemotherapy regimens for advanced non-Hodgkin’s lymphoma. N Engl J Med 328:1002-1006, 1993.
- Meignan M, Gallamini A, Meignan M, et al: Report on the first International Workshop on Interim-PET-Scan in Lymphoma. Leuk Lymphoma 50:1257-1260, 2009.
- Kurtz DM, Scherer F, Jin MC, et al: Circulating tumor DNA measurements as early outcome predictors in diffuse large B-cell lymphoma. J Clin Oncol 36:2845-2853, 2018.
- Meignan M, Cottereau AS, Versari A, et al: Baseline metabolic tumor volume predicts outcome in high-tumor-burden follicular lymphoma: A pooled analysis of three multicenter studies. J Clin Oncol 34:3618-3626, 2016.
Dr. Cheson is a hematologist/oncologist in Bethesda, Maryland.

