A new clinical guideline from the American Society for Radiation Oncology (ASTRO) provides recommendations for radiation therapy to treat patients with nonmetastatic cervical cancer. The guideline—ASTRO's first for cervical cancer—outlines indications and best practices for external-beam radiation therapy (EBRT) and brachytherapy in the postoperative and definitive settings. Recommendations also address other treatments, including chemotherapy and surgery when used in combination with radiation. The guideline was published by Chino et al in Practical Radiation Oncology.
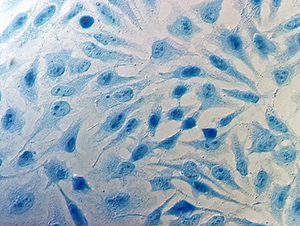
Photo credit: Getty
“[Treatment for] cervical cancer has advanced dramatically over the last 20 years. Increased use of intensity-modulated radiation therapy (IMRT) and image-guided brachytherapy, in particular, have resulted in better patient outcomes and fewer treatment complications. Our intention in developing this guideline is to encourage physicians to make these approaches part of their daily practice,” said Akila N. Viswanathan, MD, MPH, Chair of the guideline task force and Professor and Interim Director of Radiation Oncology and Molecular Radiation Sciences at the Johns Hopkins Sidney Kimmel Cancer Center.
Radiation is an integral part of cervical cancer treatment, either following surgery for patients at risk of recurrence or as a primary definitive treatment. The regimen involves pelvic EBRT, often combined with chemotherapy and a brachytherapy boost.
“We've moved from 2D and 3D treatments for the pelvis into IMRT, a highly focused form of radiation that reduces a patient's risk of treatment complications. We also have seen significant improvements in outcomes with image guidance for brachytherapy. Treatment teams use the most advanced imaging modalities available, and that allows us to treat exactly what we need to treat and avoid normal tissues,” said Junzo Chino, MD, Vice Chair of the guideline task force and Associate Professor of Radiation Oncology at Duke University Cancer Center.
The guideline was based on a systematic literature review of articles published from January 1993 through October 2018; rare histologies, noninvasive disease, and palliative treatment were outside the scope of the current guideline. The multidisciplinary panel included radiation oncologists, a gynecologic oncologist, a medical oncologist, a radiation oncology resident, a medical physicist, and a patient representative. The guideline was endorsed by the American Brachytherapy Society, Canadian Association of Radiation Oncology, European Society for Radiotherapy and Oncology, Royal Australian and New Zealand College of Radiologists, and the Society of Gynecologic Oncology.
The guideline's recommendations address the indications for postoperative and definitive radiation therapy, the use of chemotherapy in combination with radiation, the use of IMRT, and the indications and techniques of brachytherapy. Key recommendations are reproduced below.
Recommendations: Radiation Therapy for Locally Advanced Cervical Cancer
- In the postoperative setting following radical hysterectomy, radiation with concurrent platinum-based chemotherapy (chemoradiation) is recommended for patients with high-risk factors, such as positive margins. Postoperative radiation therapy is recommended for patients with intermediate-risk factors, such as larger tumors. Risk criteria are defined in the guideline.
- In the definitive setting, chemoradiation therapy is recommended for patients with International Federation of Gynecology and Obstetrics stage IB3–IVA disease. Definitive radiation or chemoradiation is conditionally recommended for patients with stage IA1–IB2 disease who are medically inoperable.
- IMRT is recommended for postoperative EBRT and conditionally recommended for definitive EBRT to reduce short- and long-term toxicity.
- Brachytherapy is strongly recommended for patients receiving definitive radiation or chemoradiation. Neither SBRT nor IMRT is a suitable substitute for brachytherapy. In the postoperative setting, brachytherapy is conditionally recommended with the presence of positive margin(s).
- The guideline also addresses optimal dosing, fractionation, and technique for EBRT and brachytherapy, including recommendations for image guidance, volume-based treatment planning, and strategies to limit radiation spread to organs at risk.
Treatment-Related Side Effects
Treatment for cervical cancer can be a challenging experience for patients, given the proximity of the cervix to other critical organs in the pelvis and the combination of multiple therapies.
“Irrespective of the techniques used, radiation therapy for cervical cancer causes side effects for many patients—most commonly, fatigue and complications in the bowel and bladder. Newer radiation technologies can significantly reduce these complications, however. The hallmark of [guided] brachytherapy, for example, is fewer bowel or bladder side effects than with traditional brachytherapy techniques. Medications to manage side effects have also improved considerably,” said Dr. Viswanathan.
“The issues facing women with cervical cancer are unique,” said Dr. Chino. “Doing everything we can to eliminate the tumor is only part of our job. The other part is to make sure that patients are doing well throughout the treatment process.”
COVID-19 and Cervical Cancer
The guideline was completed before the pandemic and therefore does not address the role of COVID-19 in the treatment of cervical cancer. Dr. Viswanathan and Dr. Chino also expressed concern about the effects of the coronavirus pandemic on patients with cervical cancer.
“Cervical cancer is one of those cancers where you just can't wait. You need to treat it right away in order to have the greatest chance of cure,” said Dr. Viswanathan.
“I worry about women not coming in at a time when earlier treatment could be exceedingly beneficial to them,” added Dr. Chino. "I hope that women who have symptoms will continue to be identified early and come in for treatment. We are also preparing for a potential surge of cases where, for understandable reasons, they did not seek screening or treatment as early as they may have before the pandemic. I fear that we will see more patients with more advanced disease.”
Both doctors noted that their clinics implemented a series of safety enhancements and process upgrades that have allowed them to continue cervical cancer treatments safely during the pandemic.
Disclosure: For full disclosures of the guideline authors, visit practicalradonc.org.

