The incidence of colorectal cancer among adults younger than age 50 has risen more than 50% over the past 25 years. Researchers are attempting to understand this phenomenon, as described in several studies presented at the 2020 Gastrointestinal Cancers Symposium that offered new insights.
Sociodemographic Disadvantages Confer Worse Survival
Lower income and educational levels can compromise survival among young adults with colorectal cancer. Such individuals present with more advanced disease. They also have worse survival, as do those living in urban/rural communities vs metropolitan areas, compared to their less disadvantaged peers, according to a retrospective cohort study based on the National Cancer Database for the years 2004 through 2016.1

“To try to eliminate these disparities, the first step is recognition.”— Ashley Matusz-Fisher, MD
Tweet this quote
The investigators analyzed 26,768 patients diagnosed with colorectal cancer between 18 and 40 years of age. Rural, urban, or metropolitan status was ascertained for 25,861 patients, and 7,743 were determined to be either low income/education or high income/education.
“Among young adults with stage IV disease, overall survival was worse in those with lower compared to higher income and education, and regardless of income and education, patients in urban and rural areas seemed to have a higher risk of death than those in metropolitan areas,” said Ashley Matusz-Fisher, MD, of the Levine Cancer Institute in Charlotte, North Carolina.
After adjustments for race, insurance status, stage of cancer, and comorbidities, individuals living in areas with low income (< $38,000 annually) and with low educational attainment (high school graduation rate < 79%) had a 24% increased risk of death (hazard ratio [HR] = 1.24; P = .004); those living in urban or rural areas vs metropolitan areas had a 10% higher risk (HR = 1.10; P = .02), she reported.
In the univariable analysis, patients in the low-income and low-education strata were six times more likely to be black and to lack private health insurance. They also had significantly more comorbidities, higher pathologic stage at diagnosis, more nodal involvement, more rehospitalization within 30 days, and were significantly less likely to undergo surgery.
Among patients with stage IV disease, the median overall survival was 26.1 months for those in high-income, high-education areas, but 20.7 months for those from low-income, low-education areas (HR = 1.4; P < .0001).
Dr. Matusz-Fisher speculated that limited access to care, lack of awareness of symptoms, and inability to afford necessary treatment may be root causes. “To try to eliminate these disparities, the first step is recognition,” she noted.
“Therefore, more effort to increase awareness regarding healthcare disparities is warranted to provide access, remove barriers to care, and not only provide equally effective treatment to all patients but hopefully deliver first-class health care to all patients’ doorsteps, regardless of where they live, to eliminate disparities and achieve health equity,” said senior study author, Mohamed E. Salem, MD, gastrointestinal oncologist and Associate Professor of Medicine at Levine Cancer Institute in Charlotte, North Carolina.

Mohamed E. Salem, MD

William Worrilow
Older vs Newer Era
A companion analysis of the National Cancer Database—which was carried out by the same group and presented at the meeting by Dr. Salem and William Worrilow of Levine Cancer Institute, Atrium Health, Charlotte, North Carolina—evaluated patient characteristics and outcomes achieved in an older era (2004–2009) and newer era (2010–2015).2 “We believe this is the first study looking at changes in young adults (< 40 years old) with colorectal cancer over time, and we found that the clinical features of colorectal cancer are changing. These findings might help us better understand the change in disease biology in these young individuals,” the investigators said.
In recent years, more diagnoses have been made in “very young” patients (aged 18–30 years; 21% vs 19%; P < .0001) but with less metastatic disease (15% vs 18%; P < .001) or nodal involvement (55% vs 58%; P < .001) at presentation. After 2010, more patients have had comorbidities (9% vs 7%; P = .0012), left-sided tumors (77% vs 76%; P = .04), and well-differentiated histology (12% vs 8%; P < .0001).
“The good news is that the overall survival for young adults presenting with stage IV disease is actually better,” they said. Median overall survival was 24.1 months in the recent cohort vs 22.5 months in the older group (P = .014). The 15% greater risk of 5-year all-cause death (P = .0001), the investigators noted, was “unexpected.”
Racial Distribution Differs by Age of Onset

Dhruvika Mukhija, MD
An analysis of the Surveillance, Epidemiology, and End Results database found that racial distribution in persons with colorectal cancer differs significantly among patients younger than age 45 as compared to those ≥ 45 years, researchers from Northwestern University, Chicago, reported.3 Young American Indians and Alaska Natives are almost twice as likely to develop colorectal cancer as their older counterparts, and blacks and Asians/Pacific Islanders are 1.5 times as likely.
“We studied 453,019 patients with colorectal cancer and compared outcomes of those above and below the age of 45. We found that among patients younger than age 45, the racial distribution of colorectal cancer was very different from those older than 45,” said Dhruvika Mukhija, MD, a fellow in hematology/oncology (Table 1).
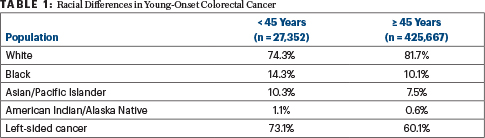
Median survival was poorer for nonwhite patients (94 months) than white patients (153 months) overall and individually for both those < 45 and those ≥ 45 years. “Nonwhite races overall had poor survival across all age groups,” Dr. Mukhija said.
“Clearly, there are risk factors for younger-onset colorectal cancer, but we don’t yet know them. With rates of colorectal cancer rapidly increasing among young adults, we believe that these demographic differences with racial disparities are extremely important to highlight. The focus of screening programs should be even more on the minority population, and we should make all efforts to increase awareness regarding this,” she said.
DISCLOSURE: Drs. Matusz-Fisher, and Mukhija and Mr. Worrilow reported no conflicts of interest. Dr. Salem has served as a consultant or advisor for Exelixis and Taiho Pharmaceutical; serves on speakers bureaus for Caris Life Sciences, Genentech/Roche, Taiho Pharmaceutical; and has received funds for travel, accommodations, or other expenses from Caris Life Sciences.
REFERENCES
1. Matusz-Fisher A, Trufan SJ, Kadakia KC, et al: Sociodemographic disparities in young adults with colorectal cancer: Analysis of 26,768 patients in the National Cancer Database. 2020 Gastrointestinal Cancers Symposium. Abstract 13. Presented January 25, 2020.
2. Trufan SJ, Worrilow WM, Kadakia KC, et al: Change of clinical features and outcomes of adolescents and young adults with colorectal cancer over time: Pooled analysis of 26,768 patients in the National Cancer Database. 2020 Gastrointestinal Cancers Symposium. Abstract 256. Presented January 25, 2020.
3. Mukhija D, Nagpal S: Impact of race on incidence and survival from colorectal cancer in young adults in the United States. 2020 Gastrointestinal Cancers Symposium. Abstract 62. Presented January 25, 2020.

