In a National Institutes of Health study reported in the Journal of Clinical Oncology, Zacharakis et al found that treatment with autologous tumor-infiltrating lymphocytes (TILs) reactive to mutations in metastatic lesions produced responses in patients with metastatic breast cancer.
Study Details
In the study, 42 women treated at the Surgery Branch of the National Cancer Institute with disease refractory to previous lines of treatment underwent surgical resection of a metastatic lesion(s), isolation of TIL cultures, identification of exomic nonsynonymous tumor mutations, and immunologic screening for neoantigen reactivity. Eligible patients with sufficient reactivity were entered into a cohort of an ongoing phase II pilot trial of adoptive cell transfer of selected neoantigen-reactive TILs combined with up to four doses of pembrolizumab.
Key Findings
TILs were isolated and grown in culture from resected lesions of all 42 patients. Among the 42 women, 28 (67%) had TILs that recognized at least one immunogenic somatic mutation (median = 3 neoantigens per patient, range: 1–11); of these, TILs from 13 patients exhibited strong reactivity, based on measurement of T-cell activation, suitable for a trial of adoptive cell transfer.
Among the 13 patients, 5 were considered clinically ineligible for adoptive cell transfer, due to poor performance status (n = 2), brain metastasis (n = 2), and low white blood cell count. Of the eight remaining eligible patients, two received other treatment for their disease.
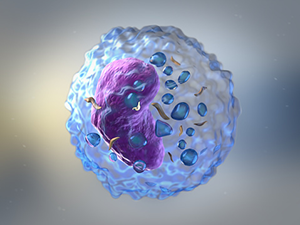
Photo credit: Getty
The remaining six patients were enrolled in the protocol of adoptive cell transfer of enriched neoantigen-specific TILs given in a single infusion in combination with four doses of pembrolizumab given every 3 weeks beginning 2 days prior to infusion. The total number of infused cells per patients ranged from 3.06e10 to 1.04e11 and were predominantly CD4-positive T cells (CD4-positive median = 56%, CD8-positive median = 37.5%). The frequency of neoantigen-reactive T cells in the infusion ranged from 10.4% to 75.2%.
Among the six patients, objective response was observed in three, including complete response in one. The patient with complete response received 1.85e10 TILs against four neoantigens and exhibited complete regression of metastatic tumors in the liver, lymph nodes, and mediastinum. Response is ongoing after 66 months.
One patient, who received 7.2e10 TILs against 10 neoantigens, had a partial response (69% reduction in tumor burden) that lasted for 10 months; the patient exhibited complete regression of widespread subcutaneous disease in the left breast and left supraclavicular and right axillary lymph node lesions, as well as a decrease in a nontarget lung tumor.
Another patient, who received 4.7e10 TILs against three neoantigens, had a partial response (52% reduction) lasting for 6 months; the patient exhibited complete resolution of two right subpectoral lymph nodes and subcutaneous breast nodules, as well as substantial regression of the right breast primary tumor.
A fourth patient, who received 4.5e10 TILs against 10 neoantigens, exhibited substantial regression of visceral disease but did not achieve objective response. Continuous regression of five liver metastatic lesions and one hilar lymph node was observed over 5 months, with complete regression of three other hilar lymph nodes. Although the responses constituted a maximum reduction of 60% from baseline tumor burden, preexisting and new metastatic bone deposits progressed or appeared within 3 months after TIL treatment.
The investigators concluded, “Most patients with breast cancer generated a natural immune response targeting the expressed products of their cancer mutations. Adoptive transfer of TIL is a highly personalized experimental option for patients with metastatic breast cancer shown to be capable of mediating objective responses in this pilot trial and deserves further study.”
Steven A. Rosenberg, MD, PhD, of the Surgery Branch, National Cancer Institute, is the corresponding author for the Journal of Clinical Oncology article.
Disclosure: The study was supported by the Center for Cancer Research at the National Cancer Institute. For full disclosures of the study authors, visit ascopubs.org.

