For patients with high-risk myeloid malignancies undergoing allogeneic hematopoietic stem cell transplant, adding the BCL-2 inhibitor venetoclax to a reduced-intensity drug regimen prior to transplant is safe and does not impair the ability of the donor cells to engraft. The phase I study was presented by Garcia et al at the 2019 American Society of Hematology (ASH) Annual Meeting & Exposition (Abstract 258).The findings provide support for the use of venetoclax prior to transplant as a way to increase the chances of transplant success in this group of patients, said first study author Jacqueline S. Garcia, MD, of Dana-Farber Cancer Institute.
“We found that venetoclax can be safely added to standard reduced-intensity conditioning without impeding the ability of donor neutrophils to engraft."— Jacqueline S. Garcia, MD
Tweet this quote
While a donor stem cell transplant can cure myeloid malignancies such as acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS), patients whose tumor cells carry certain genetic mutations or chromosomal abnormalities have a high risk of relapsing after transplant. A variety of approaches to lowering the chance of relapse are under study. One involves using venetoclax, which prompts cancer cell death by blocking the BCL-2 protein, as part of the conditioning regimen patients receive in preparation for a donor stem cell transplant.
Study Details
The new study focused on patients who underwent reduced-intensity conditioning regimens, which use lower, less toxic doses of chemotherapy and radiation therapy. While such regimens kill fewer cancer cells than traditional myeloablative treatments, they are milder on the body and are used in patients over age 60.
“In previous research, we have shown that adding venetoclax to leukemia drugs produces a very large increase in antileukemia activity,” said Dr. Garcia. “We hypothesized that venetoclax would promote the antileukemic effect of conditioning chemotherapy and therefore reduce the risk of relapse without producing undue toxicity.”
The study involved nine patients with high-risk AML or MDS who were recommended for a donor stem cell transplant. In the phase I clinical trial, they received venetoclax along with fludarabine and busulfex as a conditioning regimen, and then underwent a donor stem cell transplant.
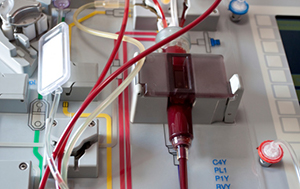
Photo credit: Getty
Results
“We found that venetoclax can be safely added to standard reduced-intensity conditioning without impeding the ability of donor neutrophils to engraft,” said Dr. Garcia.
Because patients are 6 months removed from transplant, it is too early to know if the new regimen reduced the chance of relapse, Dr. Garcia noted, but the fact that the donor cells have engrafted—evidenced by patients’ blood counts—may be an encouraging sign. There has not been a signal of toxicity in excess of what is expected with standard reduced-intensity conditioning, including rates of graft-vs-host disease.
To further minimize the potential for relapse, the trial is under an amendment to allow trial participants to receive posttransplant maintenance therapy of low-dose venetoclax plus azacitidine.
Disclosure: For full disclosures of the study authors, visit ash.confex.com.

