In a letter to the editor published in The New England Journal of Medicine, Bagchi et al describe the course of treatment in a 3-year-old child with an intracranial tumor and his response to therapy with the kinase inhibitor lorlatinib.
Key Points
Magnetic resonance imaging (MRI) of the head in a 3-year-old boy who presented with obtundation after a 2- to 3-week history of vomiting, excessive sleepiness, and exotropia revealed a large tumor in the left cerebral hemisphere.
Three attempts at surgery, the last following neoadjuvant chemotherapy, were halted due to life-threatening intracranial bleeding, with only a partial resection being performed. Further attempts at intervention were considered futile. A do-not-resuscitate order was instituted, and the child received comfort measures. However, despite removal of life support, the child’s breathing and vital signs normalized.
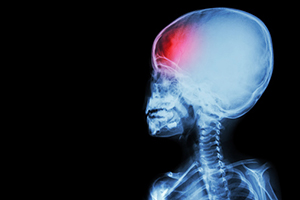
Photo credit: Getty
Neuropathology showed a high-grade astrocytic tumor diffusely immunoreactive for ALK, with methylation profiling showing a tumor of the infantile hemispheric glioma class and RNA sequencing revealing a SPECC1L-ALK fusion. Given the presence of the ALK fusion, lorlatinib was selected for treatment, based on promising intracranial responses reported with its use in adults with non–small cell lung cancer.
Treatment was started with administration of 95 mg/m2 once daily via nasogastric tube, with the dose selected based on the amount used in a previously reported pediatric refractory neuroblastoma cohort. The patient exhibited rapid signs of recovery, with neurologic function returning along with tumor shrinkage. The most prominent adverse reaction was weight gain, which persisted despite a 20% dose reduction.
MRI after 8 months of treatment showed that only a small residual tumor remained, with tumor being replaced by cystic structures. The tumor cavity was cleared in exploratory surgery, with a gross total resection being achieved.
Comparison of histologic findings before and after lorlatinib treatment showed a marked decrease in tumor proliferative index, consistent with a drug-induced response. The SPECC1L-ALK fusion was detected at low allele frequency with repeat RNA sequencing. Lorlatinib was stopped when postsurgical MRI revealed absence of tumor.
Six months after stopping treatment, the child developed facial palsy and metastatic lesions were found on cranial nerve VII and the spine. Lorlatinib treatment was restarted at an oral dose of 95 mg/m2 once daily. A rapid response was again observed, with palsy resolving within 1 week of starting treatment. MRI after 1 month of treatment showed near-complete response in all lesions.
At the time of writing, the child continued to receive lorlatinib therapy and was attending preschool with no appreciable neurologic deficits or complications from surgery. Adverse reactions were limited to grade 2 weight gain and grade 1 hypercholesterolemia.
As stated by the investigators, “Given the patient’s young age and the recent recurrence, we plan to continue therapy, absent any serious side effects, for as long as the disease remains controlled, so that more-damaging chemotherapy or radiation can be avoided or delayed.”
They concluded, “ALK inhibitors biochemically developed to penetrate the central nervous system, such as lorlatinib, can affect primary tumors of the central nervous system that harbor target lesions and warrant investigation in the management of ALK-fused glioma.”
Giles W. Robinson, MD, of St. Jude Children’s Research Hospital, is the corresponding author for The New England Journal of Medicine letter.
Disclosure: The work was supported by the American Lebanese Syrian Associated Charities and a grant from the National Cancer Institute. For full disclosures of the study authors, visit nejm.org.

