
Vincent T. DeVita, MD

George P. Canellos, MD
Medical oncology had a turbulent beginning. No other specialty we know of struggled as much. But by 1980, it had become a stable specialty of internal medicine and was off and running—with the major problem of how to marshal available resources to freely test the myriad opportunities presented by combination chemotherapy, immunotherapy, and targeted therapy, especially if used together in novel ways.
The main source of the rough and tumble was the prevailing attitude in academia in the 1950s and 1960s that if you couldn’t remove a localized cancer one way or another, cancer was a death sentence. In truth, this
attitude was not surprising. There wasn’t much that could be done for patients with advanced cancer for most of the 20th century except to make patients as comfortable as possible and to ease their way into the world beyond.1
There was a self-fulfilling prophecy that was born of this attitude, though, which impeded any attempts to try and find new treatments. “Advanced cancer is incurable; if it’s incurable, why treat it? And then indeed it is incurable.” Unless or until it could be shown that cancer could be cured by systemic treatment, the field could go nowhere.
That proof of principle was provided by the cure of childhood acute lymphocytic leukemia (ALL) and advanced Hodgkin lymphoma (HL) with combination chemotherapy and with the early success of the adjuvant treatment of resected breast cancer.
In this piece, we will showcase the results of the pivotal studies that actually moved the needle toward cure. In each case, they were, by consensus, landmark studies, producing first-of-their-kind results. The fact that many of the studies emanated from the National Cancer Institute’s (NCI’s) Medicine Branch was no accident. It happened because a collection of highly motivated people were supplied with a largesse of funds and tools never before assembled in one place to do clinical research. At the time, there simply was no other place in the country with access to funding and all the critical tools, in a permissive environment, where these types of studies could have been done.
Three Key Events
Let’s start at the beginning. Three major events occurred at the turn of the 20th century that had a significant impact on the development of cancer therapeutics and the specialty of medical oncology: the discovery of x-rays, the development of the Halsted radical mastectomy, and the availability of transplantable animal tumors in inbred strains of mice.1
Diagnostic radiology departments absorbed the new field of therapeutic radiology; for decades, they coexisted in stable single departments and then as independent departments, as the tools of their trade continuously improved from kilowatt machines to linear accelerators to proton beam systems.
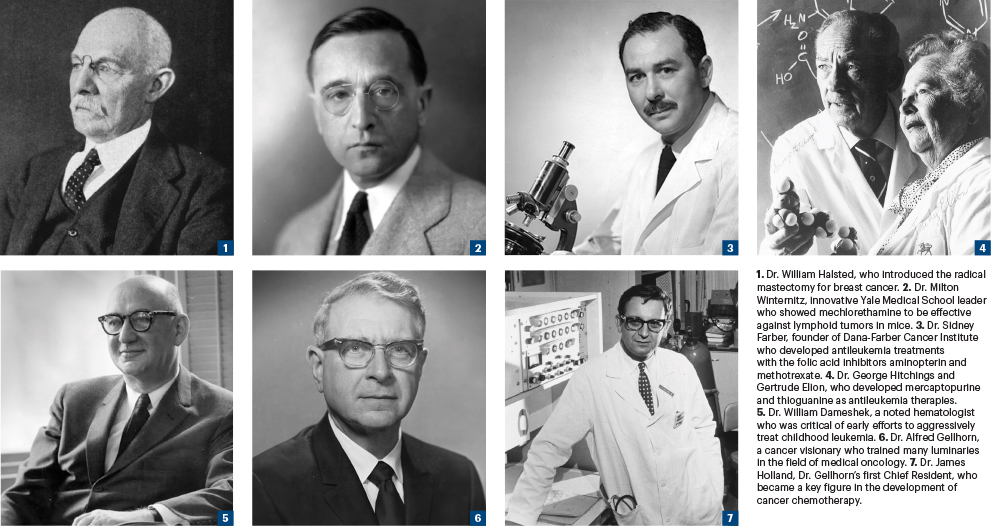
The radical mastectomy was based on Dr. William Halsted’s contention that cancers spread by marching directly into adjacent tissue and that tissue needed to be removed surgically by “en bloc resection”—all involved tissue in one piece. Dr. Halsted used this approach even if a patient had adjacent bone involvement.
The en bloc resection came to be known as “the cancer operation” and was applied whenever possible to all tumor types. And thus, a subgroup of surgeons who specialized in cancer surgery using en bloc resections came to exist in departments of surgery. The procedure was applied with gusto in breast cancer, and the radical mastectomy would be the main treatment of localized breast cancer for 75 years, even though Dr. Halsted’s hypothesis of spread had long been proven wrong. It was both too much and too little—too much for small tumors and too little for big tumors. As time went on and the use of combined-modality treatments emerged, cancer surgery evolved into tailoring operations to fit the peculiarities of the other modalities.
Both radiotherapy and the cancer operation were seen as the treatments of choice for all types of localized cancer. Cross-collaboration between surgery and therapeutic radiology was minimal at first, as both specialties instead pursued applying their tools more aggressively. Giving cancer drugs after surgery or radiotherapy, when there was no proof that they could cure anyone, was not an option in practice.
For advanced cancers, there was not much available in terms of treatment, although hormone therapy in prostate and breast cancers came on the scene when Charles Huggins, MD, described alterations of the course of the diseases by hormones in 19412 and won the Nobel Prize for his work in 1966. But although this approach is always useful, it is almost never curative.
Some physician scientists dreamed of developing drugs—“silver bullets”—that might eradicate cancer. Still, how to identify and apply such agents was a problem. Few believed it was possible. But some did.
It was George Clowes, MD, at Roswell Park Cancer Institute in Buffalo, New York, in 1912, who developed transplantable tumors in inbred mice into a system that would allow the screening of chemicals against rodent tumors.3 Unlike en bloc surgery and the use of radiation to treat cancer, there was no immediate medical home for screening systems. For the next 30 years, laboratory investigators of all persuasions, all over the world, developed their own transplantable tumor systems, vying for the one that everyone could use that would reliably predict a chemical would work against human cancers, without much success. This was mainly because there were few matching clinical cancer programs available, or specialized clinicians, to test cancer drugs in an organized way.
Ultimately, in 1955, the drug development program at the NCI did select a carcinogen-induced lymphoid leukemia, developed by NCI geneticist Lloyd Law, PhD, as its universal screen. It was named Leukemia 1210, or L1210 for short. It soon became the most common starting point to screen new chemical structures for antitumor activity, largely because L1210 predicted activity of all known active antitumor agents at the time.4 The first anticancer drugs, however, were not discovered in formal screens but by accident, by using ad hoc screening systems or intuitively.
It took World War II and the advent of the U.S. gas warfare program to focus the attention of investigators on the depleting effects of mustard gas on the bone marrow and lymphoid system in soldiers exposed to mustard gas during an incident in Bari Harbor in Italy.5 Similar effects had been seen in gas-exposed soldiers in World War I but largely ignored.6
A derivative of mustard gas, nitrogen mustard (now known as mechlorethamine), was synthesized and was shown to be effective when tested against lymphoid tumors in mice at Yale in 1943 by Milton Winternitz, MD, who was under contract with the U.S. Office of Scientific Research and Development to test it. Gustaf Lindskog, MD, a thoracic surgeon at Yale, tested mechlorethamine in a single very ill patient with lymphoma in 1943, achieving an initial dramatic response, although the patient ultimately relapsed and died of his disease.5 Because of the secrecy surrounding the gas warfare program, this work was not published until 1946, and it caused quite a stir since it suggested a chemical might cure advanced cancer.7
First Trials of Anticancer Drugs in Humans
Multiple single-institution clinical studies of mechlorethamine were started in the late 1940s and early 1950s, all with essentially the same results—brief clinical responses lasting a few months, invariably followed by relapse, with even less useful responses on retreatment. This caused great gloom among physicians who did the early testing.
In rapid succession, five more anticancer drugs were developed at single institutions where researchers had access to clinical facilities to test their effects in humans. Sidney Farber, MD, and colleagues developed the folic acid inhibitors, aminopterin and methotrexate.8 George Hitchings, PhD, and Gertrude Elion, MSc, discovered two compounds that inhibited adenine metabolism that were effective in rodent leukemia.9 By 1951, they brought mercaptopurine and thioguanine to market.
The last of the five was intuitively developed by Charles Heidelberger, PhD, at the University of Wisconsin.10 He had noted that hepatomas in mice had greater uptake of uracil than surrounding normal liver and decided to “target” this difference by attaching a fluorine atom to the 5 position of the uracil base. By the mid-1950s, the compound fluorouracil (commonly known as 5-FU) became available for clinical use providing the first example of a specifically targeted therapy. Fluorouracil differed from the previous antimetabolites in that it had a spectrum of activity against solid tumors, whereas the others seemed only effective against lymphoid leukemias. Unfortunately, responses to fluorouracil were brief, relapse was invariable, and toxicity was severe.
Corticosteroids initially used to treat rheumatoid arthritis were also found to be useful in lymphoid tumors in the 1950s. These agents produced brief remissions in leukemia with a toxicity profile different from the new cytotoxics.11
Early Days of Chemotherapy—and Its Critics
With tools now available to treat advanced cancer, a cadre of physicians in cancer hospitals all over the world began to use them. Many of these physicians were located in departments of medicine in medical schools. Since there were no training programs for these cancer doctors, and most had been trained in other areas of internal medicine, administering anticancer drugs was self-taught and considered a sideline. They were called chemotherapists.
The results of these treatments were dismal and widely derided in the academy. Giving anticancer drugs to patients with cancer was not considered a viable pathway to promotion. And a new breed of critics was born.12
William Dameshek, MD, a famous hematologist, whose early efforts with mechlorethamine had failed, devoted the agenda of The Blood Club, a group of distinguished hematologists who met annually in Atlantic City, to trashing the investigators trying to aggressively treat childhood leukemia.
Some investigators lost their positions. At the Delafield Hospital, one of the oldest cancer hospitals in New York City, Alfred Gellhorn, MD, Director of Delafield, trained as a surgeon and self-taught in treating cancer patients with drugs, was asked to leave because the Chairman of Medicine had an aversion to exposing his house staff to the fruitless task of treating dying patients with cancer. The hospital was closed. Dr. Gellhorn once told one of us (VTD) that on rounds, in front of residents and fellows, the Chairman was fond of saying “Alfred, you are part of the lunatic fringe.” Not a good recommendation for climbing the academic ladder. Nevertheless, the doctors Dr. Gellhorn trained turned out to be a who’s who of medical oncology in later years. His first Chief Resident was James Holland, MD.
At the clinical center of the NCI, where the authors worked, a distinguished hematologist, George Brecher, MD, who read all the bone marrow slides from the leukemia service, referred to the service as “the butcher shop.” Hematologists remained unenthusiastic about adopting anticancer drugs or the doctors who administered them.
Charles Moertel, MD, a gastroenterologist by training from the Mayo Clinic, spent his entire career trying to prove that fluorouracil didn’t work in patients with colorectal cancer and should be removed from the market. He was wrong. Today, it remains a mainstay of the treatment of colorectal cancer, just not by itself.
Most doctors, like Dr. Moertel, felt that sick patients with cancer didn’t need to be made sicker by administering drugs that produced a wide array of unique, serious toxicities when not a single study showed clear evidence of prolongation of life. The self-fulfilling prophecy was at work.
The discontent at many academic institutions often started with house officers who were uncomfortable taking care of dying patients with cancer to begin with (as some were their own age) and thought testing new drugs in dose-finding studies was unethical, since no beneficial therapeutic effects were anticipated. These patients were human guinea pigs, they said. And indeed they were, although with their permission.
Foundations of the Specialty
The 1950s were chaotic. Yet the groundwork and tools of the trade of what became the specialty of medical oncology were laid down in that decade.
In 1953, the clinical center of the National Institutes of Health (NIH) opened. It had about 200 beds, and each of the separate institutes of the NIH were allocated a portion of the beds, which they would be required to staff with doctors themselves. The NCI, the largest of the institutes, had roughly 100 beds divided among the clinical branches. The two sections of the Medicine Branch, where most of the chemotherapy work was done—the leukemia service and the solid tumor service—had 26 beds each.
This was not to be your ordinary hospital. It was designed to be a special place and do special things, which it ultimately did. Ratcheting ahead 10 years, the clinical branches were by then honed into ideal instruments for clinical research. Admission was free to patients involved in research. There were no restrictions on length of stay.
Studies testing new therapies are best done on previously untreated patients. They were difficult to come by in the NCI catchment area. By the time the authors arrived in 1963, the NCI had solved the problem by providing free transportation for patients who were referred from afar in response to ads in medical journals and free housing in a local motel for the patient and his or her family, if needed.
But Where to Get the Best and Brightest Physicians?
NIH was part of the Department of Health and Human Services (HHS). The Public Health Service (PHS) was part of HHS, and PHS staff were considered part of the uniformed services. Doctors who were accepted to any NIH institute could satisfy their required military service. They could also get research experience that would make them attractive to programs at major research universities after they left NIH, and many populated university cancer programs for decades after they served their time at NCI. Intramural staff also did not need to apply for grants to fund their research; it was all supported by part of the NCI allocation.
The Vietnam War was raging, and doctors were being drafted right out of training. Physicians began to apply in droves for NIH Clinical Associate positions (the equivalent of a fellowship at a university) to avoid the draft. One year, we had 1,100 applications for our 14 positions. We could pick and choose the best and brightest graduates who had, at a minimum, completed a year of internship.
We had the formula for success—a permissive environment, bright young physician-scientists, financial support, and access to all the newest tools of the trade necessary to do ideal clinical research.
Further Organizational Growth
In 1954, C. Gordon Zubrod, MD, arrived from Saint Louis University to be Clinical Director of the NCI. Dr. Zubrod had been a Distinguished Professor at Johns Hopkins University and had been involved in the U.S. gas warfare program in the Office of Scientific Research and Development.
In 1955, Dr. Zubrod, in turn, hired Emil Frei III, MD (known to friends and colleagues as Tom), who he knew from St. Louis, to be Chief of the Medicine Branch. The brilliant Emil J Freireich, MD (known to friends and colleagues as J) applied for a position to escape the draft. And the famous duo of Frei and Freireich was born. Dr. Zubrod’s instruction to Drs. Frei and Freireich was to try to find a cure for childhood acute leukemia.
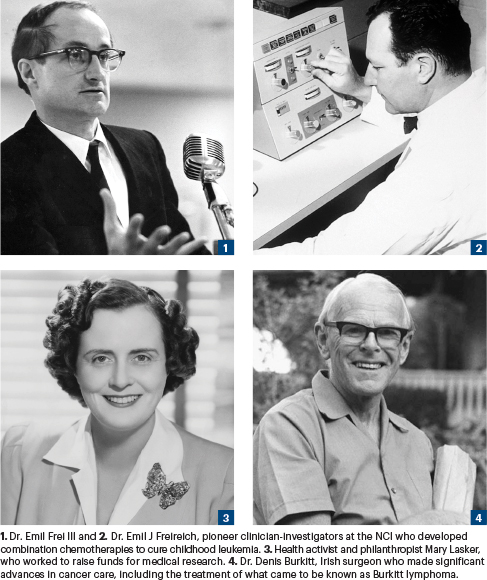
In 1955, the Cancer Chemotherapy National Service Center (CCNSC) was established.13 The philanthropist Mary Lasker, impressed by the success of the WW II antimalarial drug program, the availability of new cancer drugs, and the early results in childhood leukemia with methotrexate reported by her friend Sidney Farber, MD, convinced the U.S. Congress to award the NCI $5 million to establish a cancer drug discovery and development program.
The CCNSC was born 18 months later, under the tutelage of Ken Endicott, MD, head of the chemotherapy research program at NCI. It not only set up a screening program based on the L1210 model but contracted with institutions around the world for the production of mice, to perform the screening services, to do toxicology studies on drugs that passed decision points indicating potential clinical use, and to provide services to synthesize and produce chemical structures of interest.
It also became a worldwide program. An extension of the drug screening program was eventually set up and managed by an NCI office in Brussels. And the initial support for the European Organisation for Research and Treatment of Cancer (EORTC), a cooperative clinical trials program that grew into a central treatment development program in Europe, came from this program.
With increasing collaboration with the Istituto Nazionale dei Tumori in Milan, the NCI provided funds to establish a clinical trials office to support their studies in breast cancer and lymphoma. These programs played a significant role in the emergence of medical oncology as a specialty in Europe.14 With a formal program to nurture and sustain drug development, a new Division of Chemotherapy was established at NCI under the leadership of Dr. Zubrod, as Dr. Endicott became NCI Director.
Dr. Zubrod, an unsung hero in the field, organized a special task force on clinical trials that revolutionized clinical studies by outlining the phases of clinical trials to develop new treatments or evaluate new drugs—phases I, II, and III, still used today—and the introduction of statistics to protocol development. For phase III studies, comparing new treatments with old ones, he introduced the newly described randomized clinical trials.3,15 He brought order to clinical studies and financial support for large-scale randomized clinical trials under the umbrella of clinical cooperative groups. Funds were also provided for training programs for oncologists.
The NCI drug development program, supported by research contracts, was a “from soup to nuts” program. There was something for everybody.
Two More Breakthroughs
The 1950s ended on what should have been an upbeat note, with reports of the “cure” of two more tumors that ultimately succumbed to combination chemotherapy. The first was Burkitt lymphoma, and the second, the placental tumor choriocarcinoma, both rare tumors. Both had similar unusual histories of being curable to some degree by single drugs.
Burkitt lymphoma occurred commonly in equatorial Africa.16 At first described as a sarcoma, it was later reclassified as a B-cell lymphoma. Irish surgeon Denis Burkitt, MD, reported a handful of long-term survivors with low-dose cyclophosphamide. The NCI established an outpost in Uganda in 1972 and staffed it with NCI clinical associates to study the disease, to see if there was something unusual about this tumor that led to its easy cure with a single agent—the two leading speculations were different growth characteristics and different metabolism of cyclophosphamide. One of us (VTD) spent some time studying cyclophosphamide metabolism in Burkitt patients in Uganda and found no difference in drug handling compared with American patient controls. Ultimately it was shown that Burkitt cells had a very high growth fraction resembling L1210, which probably accounted for its drug sensitivity. Later it was shown that unique use of combination chemotherapy more than quadrupled the cure rate.17
M.C. Li, MD, and colleagues reported the “cure” of metastatic choriocarcinoma with methotrexate alone.18 Their findings were met with skepticism because of the nature of the tumor, derived from both parents. The remissions were initially called spontaneous because of presumed immunologic rejection, by none other than Dr. Zubrod. Later, as with Burkitt lymphoma, standard treatment for choriocarcinoma became the use of combinations of drugs, which substantially increased the cure rate. Dr. Li’s unorthodox use of methotrexate had caused unusual anxiety among his colleagues, and he eventually had to leave the NCI.
Lingering Skepticism
It was still hazardous to be a chemotherapist, and the mood in the 1950s was gloom and skepticism about the potential of curing cancer with drugs. Chemotherapists avoided mentioning the word “cure” in their talks. Some still do.
Surgery could cure some patients with localized disease, although more aggressive surgery did not seem to improve results. Radiation therapy could also cure some patients with localized disease, but expanding the fields and increasing doses with the equipment available at the time pushed radiotherapy up against normal tissue tolerance, also without much additional benefit.
By the 1950s, it was apparent that a survival plateau had been reached with existing treatments. It was thought that the reason for this limit was that cells escaped from the primary tumor, presumably most often caused by surgical manipulation. Chemotherapy had yet to prove it could cure any common cancers in children or adults. Until it did, there was still no desire to add it to other forms of treatment to treat escaped cancer cells.
The 1960s opened with welcome news of the introduction of a new class of active cancer drugs—the vinca alkaloids, vinblastine and vincristine.19 But the leading question of the day remained: Does chemotherapy do more harm than good?
In part 2 of this two-part article, we will discuss the development of other novel protocols, the introduction of MOPP chemotherapy, and the beginnings of ASCO.
DISCLOSURE: Dr. DeVita and Dr. Canellos reported no conflicts of interest.
REFERENCES
1. DeVita VT: The evolution of therapeutic research in cancer. N Engl J Med 298:907-910, 1978.
2. Huggins C, Hodges CV: Studies on prostatic cancer: I. The effects of castration, of estrogen and of androgen injection on serum phosphatase in metastatic carcinoma of the prostate. Cancer Res 1:293-297, 1941.
3. Zubrod CG, Schepartz SA, Carter SK: Historical background for the National Cancer Institute’s drug development thrust. Natl Cancer Inst Monogr 45:7-11, 1977.
4. Law LW, Dunn TB, Boyle PJ, et al: Observations on the effect of a folic acid antagonist on transplantable lymphoid leukemias in mice. J Natl Cancer Inst 10:179-192, 1949.
5. Fenn JE, Udelsman R: First use of chemotherapy cancer treatment: Rectifying the record. J Am Coll Surg 212:413-417, 2011.
6. Krumbhaar EB, Krumbhaar HD: The blood and bone marrow in yellow gas (mustard gas) poisoning: Changes produced in bone marrow in fatal cases. J Med Res 40:497-508, 1919.
7. Goodman LS, Wintrobe MM, Dameshek W, et al: Nitrogen mustard therapy: Use of methyl-bis (h-chloroethyl) amine hydrochloride and tris (h-chloroethyl) amine hydrochloride for Hodgkin’s disease, lymphosarcoma, leukemia, and certain allied and miscellaneous disorders. JAMA 132:126-132, 1946.
8. Farber S, Diamond LK, Mercer RD, et al: Temporary remissions in acute leukemia in children produced by folic acid antagonist, 4-aminopteroyl-glutamic acid (aminopterin). N Engl J Med 238:787-793, 1948.
9. Hitchings GH, Elion GB: The chemistry and biochemistry of purine analogs. Ann NY Acad Sci 60:195-199, 1954.
10. Heidelberger C, Chaudhuari NK, Danenberg P, et al: Fluorinated pyrimidines: A new class of tumor inhibitory compounds. Nature 179:663-666, 1957.
11. Pearson OH, Eliel LP, Rawson RW, et al: ACTH- and cortisone-induced regression of lymphoid tumors in man: A preliminary report. Cancer 2:943-945, 1949.
12. DeVita VT, DeVita-Raeburn E: The Death of Cancer: After Fifty Years on the Front Lines of Medicine, a Pioneering Oncologist Reveals Why the War on Cancer Is Winnable—and How We Can Get There. New York, Sarah Crichton Books/Farrar, Straus and Giroux, 2015.
13. Cancer Chemotherapy National Service Center specifications for screening chemical agents and natural products against animal tumors. Cancer Chemother Rep 1:42-64, 1959.
14. Monfardini S, Balducci L: The history of medical oncology in Europe, 1955-1985. Part 1: Early pioneers, clinical trials, and drug development. The ASCO Post, December 10, 2021.
15. Hill AB: Randomized clinical trial of streptomycin. Brit Med J Medical Research Council, 1948.
16. Burkitt D: A sarcoma involving the jaw in African children. Br J Surg 46:218-223, 1958.
17. McGrath I: Towards curative therapy in Burkitt lymphoma: The role of early African studies in demonstrating the value of combination therapy and CNS prophylaxis. Adv Hematol. January 11, 2012 (early release online).
18. Li MC, Hertz R, Bergenstal DM: Therapy of choriocarcinoma and related trophoblastic tumors with folic acid and purine antagonists. N Engl J Med 259:66-74, 1958.
19. Johnson TS, Armstrong JG, Gorman M, et al: The vinca alkaloids: A new class of oncolytic agents. Cancer Res 23:1390-1427, 1963.
Dr. DeVita is the Amy and Joseph Perella Professor of Medicine and Professor of Epidemiology and Public Health at Yale Cancer Center. He has served as Director of Yale Cancer Center (1993–2003), Director of the NCI and the National Cancer Program (1980–1988), and President of ASCO (1977–1978). Dr. Canellos is a senior physician at Dana-Farber Cancer Institute and Brigham and Women’s Hospital. He is the former Editor-in-Chief of the Journal of Clinical Oncology (1988–2001) and President of ASCO (1993–1994).


