GUEST EDITOR

Jun J. Mao, MD, MSCE
Integrative Oncology is guest edited by Jun J. Mao, MD, MSCE, Laurance S. Rockefeller Chair in Integrative Medicine and Chief of Integrative Medicine Service at Memorial Sloan Kettering Cancer Center, New York.
Cancer and its treatments are associated with severe fatigue, depression, and sleep disturbance, which can negatively impact both physical and mental well-being. A possible contributor to these symptoms is thought to be the disruption of circadian rhythm, which regulates the sleep-wake cycle. Light therapy appears to be a promising intervention to mitigate such disruption by promoting circadian entrainment. It has been reported to be effective in reducing circadian rhythm problems associated with jetlag and depression. In this installment of The ASCO Post’s Integrative Oncology series, Dr. Redd and his colleagues summarize the research on light interventions for addressing circadian rhythm disruption in oncology settings.
Circadian Rhythm Disruption and Its Effects
Severe fatigue, depression, and sleep disturbance can be debilitating for patients with cancer. These symptoms typically develop early in the disease course and are exacerbated by treatment.1-5 They can be so severe that cancer therapies may have to be modified to make them tolerable.1 Depending on the cancer type, between 23% and 44% of survivors reportedly suffer from these sequelae for up to 5 years after all medical treatment has ended.6,7
One of the mechanisms underlying these symptoms is thought to be the disruption of circadian rhythm (ie, disruption in 24-hour cycles of hormone secretion, body temperature, and sleep-wake activity cycles, which respond to environmental cues, such as light and darkness). Circadian rhythm disruption is well documented among patients with cancer, as evidenced by impaired sleep-wake phases, flat diurnal cortisol rhythms, and lower melatonin levels in the evening during disease progression and treatment.8-10 Such disruption has also been shown to affect survival.11-13
Light Interventions for Circadian Rhythm Disruption
The focus of our research has been to determine how light can be used to promote circadian entrainment or synchronization in patients with cancer to alleviate the negative effects of circadian rhythm disruption. In the absence of external cues, the duration of the human circadian system is slightly more than 24 hours. Morning light, especially daylight, is the most effective synchronizer of the circadian system to the local time. Therefore, we delivered circadian-effective light to patients with cancer in the morning for a minimum of 30 minutes to entrain their circadian systems to alleviate the aforementioned sequelae.

FIGURE 1: Systematic light exposure, AYO light glasses.
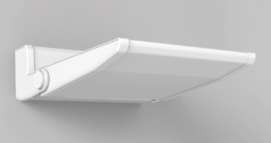
FIGURE 2: Programmed environmental illumination wall sconce.
We used two separate light delivery procedures: 1) systematic light exposure, in which circadian-effective light is projected directly onto the eyes from small portable light glasses or a light box (Figure 1), and 2) programmed environmental illumination, which provides indirect, circadian-effective illumination to the entire hospital room, either from free-standing lamps or wall sconces (Figure 2). Both procedures are comparable in circadian rhythm synchronization but differ in the ease of delivery and cost. Programmed environmental illumination places no demands on the patient, as the light is received passively, whereas systematic light exposure—the less-expensive method—requires active involvement and patients need to wear the light glasses.
For the initial efficacy trial of systematic light exposure, 34 cancer survivors who were treated for multiple myeloma, diffuse large B-cell lymphoma, breast cancer, and gynecologic cancer were enrolled. At study onset, all participants were determined to be clinically fatigued (Functional Assessment of Chronic Illness Therapy–Fatigue score > 30). They were randomly assigned to receive either bright white light or dim red light; they were instructed to self-administer treatment for 30 minutes every morning within 30 minutes of waking for 4 weeks.
At the end of the study period, those who received bright white light (circadian-effective light) had significantly less fatigue than those who received the dim red light (circadian-ineffective).14 Further data analyses revealed significant improvements in sleep efficiency as well in the circadian-effective light group, with their sleep efficiency within clinically normal range at the end of the study period and at follow-up.15
“Both programmed environmental illumination and systematic light exposure are easy to deliver, inexpensive, and safe, with the potential for improving patients’ quality of life and perhaps their medical course.”— William H. Redd, PhD, and colleagues
Tweet this quote
In another randomized trial of programmed environmental illumination involving patients with multiple myeloma (n = 187) undergoing stem cell transplantation, the prevalence of depressive symptoms was higher in patients receiving circadian-ineffective light. Two weeks after transplantation, 69.4% of patients receiving circadian-ineffective light were above the clinical threshold for depression (according to the Center for Epidemiologic Studies Depression scale). whereas 42.1% of patients receiving circadian-effective light scored above the threshold.16
We are currently investigating the mechanisms underlying the effects of light intervention on the circadian system (eg, melatonin and cortisol) and inflammatory immune markers. Our preliminary unpublished results from the study on programmed environmental illumination showed that during hospitalization, there was a steep decline in melatonin in patients in the circadian-ineffective condition, whereas the levels were relatively constant in the circadian-effective condition. This finding suggests that circadian entrainment was maintained when receiving circadian-effective light. In addition, interleukin 6, an inflammatory cytokine linked to fatigue, increased during and after hospitalization among patients receiving circadian-ineffective light. No such increase was observed in the circadian-effective light group.
Future Directions
We have immediate plans to explore the use of systematic light exposure to address three distinct problems related to disease processes: to control metabolic syndrome in patients with breast cancer who are undergoing chemotherapy, which is associated with weight gain and disease progression17; to treat frailty in elderly men undergoing hormone-deprivation therapy for metastatic prostate cancer, which is also associated with weight gain, fatigue, and disease progression18; and to improve bone health in patients with breast cancer and multiple myeloma, which are associated with bone fractures.19,20 All of these problems are linked to circadian disruption and may potentially be alleviated by light-exposure interventions.
STUDY GOALS OF LIGHT EXPOSURE IN ONCOLOGY
- To control metabolic syndrome in patients with breast cancer who are undergoing chemotherapy
- To treat frailty in elderly men undergoing hormone-deprivation therapy for metastatic prostate cancer
- To improve bone health in patients with breast cancer and multiple myeloma
In closing, both programmed environmental illumination and systematic light exposure are easy to deliver, inexpensive, and safe, with the potential for improving patients’ quality of life and perhaps their medical course. ■
Dr. Redd is Professor, Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York. Dr. Sommer is a researcher, Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York. Dr. Figueiro is the Director of The Lighting Research Center, Rensselaer Polytechnic Institute, Troy, New York. Dr. Mortimer is the Director of the Womens Cancers Program, Comprehensive Cancer Center, City of Hope National Medical Center, Duarte, California. Dr. Buettner is Professorin the Department of Medicine, Icahn School of Medicine at Mount Sinai, New York. Dr. Bailey is a Postdoctoral Research Associate in the Department of Medicine,, Icahn School of Medicine at Mount Sinai, New York. Dr. Dale is Clinical Professor in the Department of Supportive Care Medicine, City of Hope National Medical Center, Duarte, California. Dr. Winkel is a Research Professor, Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York. Dr. Valdimarsdottir is Assistant Professor, Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York.
DISCLOSURE: Drs. Redd, Sommer, Figueiro, Mortimer, Buettner, Bailey, Dale, Winkel, and Valdimarsdottir reported no conflicts of interest.
REFERENCES
1. Wang XS, Woodruff JF: Cancer-related and treatment-related fatigue. Gynecol Oncol 136:446-452, 2015.
2. Irvine D, Vincent L, Graydon JE, et al: The prevalence and correlates of fatigue in patients receiving treatment with chemotherapy and radiotherapy: A comparison with the fatigue experienced by healthy individuals. Cancer Nurs 17:367-378, 1994.
3. Macquart-Moulin G, Viens P, Genre D, et al: Concomitant chemoradiotherapy for patients with nonmetastatic breast carcinoma: Side effects, quality of life, and organization. Cancer 85:2190-2199, 1999.
4. Vogelzang NJ, Breitbart W, Cella D, et al: Patient, caregiver, and oncologist perceptions of cancer-related fatigue: Results of a tripart assessment survey. Semin Hematol 34(suppl 2):4-12, 1997.
5. Yellen SB, Cella DF, Webster K, et al: Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manage 13:63-74, 1997.
6. Shi Q, Smith TG, Michonski JD, et al: Symptom burden in cancer survivors 1 year after diagnosis: A report from the American Cancer Society’s Studies of Cancer Survivors. Cancer 117:2779-2790, 2011.
7. Savard J, Morin CM: Insomnia in the context of cancer: A review of a neglected problem. J Clin Oncol 19:895-908, 2001.
8. Innominato PF, Roche VP, Palesh OG, et al: The circadian timing system in clinical oncology. Ann Med 46:191-207, 2014.
9. Lamia KA: Ticking time bombs: Connections between circadian clocks and cancer. F1000Res 6:1910, 2017.
10. Shilts J, Chen G, Hughey JJ: Evidence for widespread dysregulation of circadian clock progression in human cancer. PeerJ 6:e4327, 2018.
11. Schrepf A, Thaker PH, Goodheart MJ, et al: Diurnal cortisol and survival in epithelial ovarian cancer. Psychoneuroendocrinology 53:256-267, 2015.
12. Sephton SE, Lush E, Deder EA, et al: Diurnal cortisol rhythm as a predictor of lung cancer survival. Brain Behav Immun 30:163-170, 2013.
13. Sephton SE, Sapolsky RM, Kraemer HC, et al: Diurnal cortisol rhythm as a predictor of breast cancer survival. J Natl Cancer Inst 92:994-1000, 2000.
14. Redd WH, Valdimarsdottir H, Wu LM, et al: Systematic light exposure in the treatment of cancer-related fatigue: A preliminary study. Psychooncology 23:1431-1434, 2014.
15. Wu LM, Amidi A, Valdimarsdottir H, et al: The effect of systematic light exposure on sleep in a mixed group of fatigued cancer survivors. J Clin Sleep Med 14:31-39, 2018.
16. Valdimarsdottir HB, Figueiro MG, Holden W, et al: Programmed environmental illumination during autologous stem cell transplantation hospitalization for the treatment of multiple myeloma reduces severity of depression: A preliminary randomized controlled trial. Cancer Med 7:4345-4353, 2018.
17. Turek FW, Joshu C, Kohsaka A, et al: Obesity and metabolic syndrome in circadian clock mutant mice. Science 308:1043-1045, 2005.
18. Piovezan RD, Poyares D, Tufik S: Frailty and sleep disturbances in the elderly: Possible connections and clinical implications. Sleep Sci 6:175-179, 2013.
19. Swanson CM, Shea SA, Wolfe P, et al: Bone turnover markers after sleep restriction and circadian disruption: A mechanism for sleep-related bone loss in humans. J Clin Endocrinol Metab 102:3722-3730, 2017.
20. Wu QY, Wang J, Tong X, et al: Emerging role of circadian rhythm in bone remodeling. J Mol Med (Berl) 97:19-24, 2019.

