An international multidisciplinary group of experts has updated their recommendations for staging and treatment response assessment in patients with Hodgkin and non-Hodgkin lymphomas. Bruce D. Cheson, MD, Professor of Medicine, Deputy Chief of Hematology-Oncology, and Head of Hematology at the Georgetown University Hospital’s Lombardi Cancer Center in Washington, DC, presented some highlights at the Pan Pacific Lymphoma Conference; the recommendations were published in their entirety in August.1
Clearer, Simpler, More Practical Guidance
The recommendations, last revised in 2007,2 are now called the Lugano Classification as they arose out of a workshop held in Lugano, Switzerland. “This will be a substantial change in how clinicians practice,” Dr. Cheson predicted in an interview. The update entailed “taking the initiative to reject some of the ways we did things in the past to try and make these new staging and response criteria more contemporary and to reflect how we actually manage patients today.”
“These recommendations will hopefully be adopted as widely as those in the past and will serve the patients better, particularly with the elimination of some unnecessary procedures; will serve the clinical research community better because these are hopefully clearer than past recommendations, and the regulatory agencies because they will now have standardized, internationally accepted staging as well as response criteria; and will better serve the pharmaceutical industry, which has always had some questions about how to interpret one thing or another,” he commented.
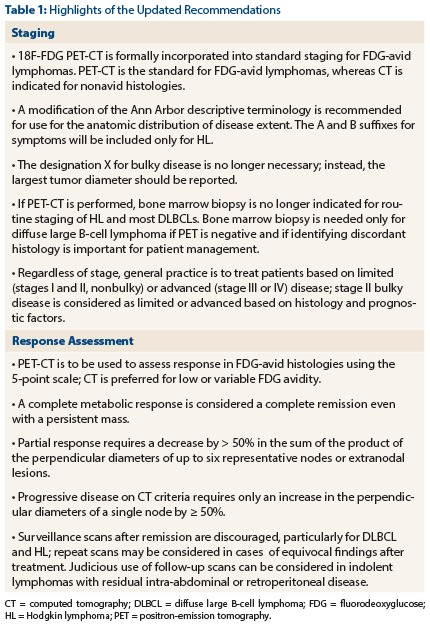
“We have modified both staging and response criteria to make them more relevant to how we currently practice hematology-oncology,” Dr. Cheson noted (see Table 1 for highlights). “We have done our best to eliminate various procedures and tests that are not necessary and may be onerous to the patient, where possible. We have clarified how you interpret response to make it easier to understand and use, and to compare study vs study. And we have better defined how to use and how to interpret positron-emission tomography (PET) scans, when to use them, when not to use them.”
Dr. Cheson said that he expected the National Comprehensive Cancer Network (NCCN) will incorporate the new recommendations into their guidelines, which some insurers use when making coverage decisions. “The last version [in 2007] was adopted by the NCCN guidelines, so I am fairly certain that this version will be as well,” he said.
Staging Recommendations
In the area of staging, “we have updated the staging criteria for lymphoma, incorporating for the first time PET for those histologies of lymphoma that are fluorodeoxyglucose (FDG)-avid,” Dr. Cheson explained. Although hematologists often obtained these scans before treatment in the past, they were not formally used in staging.
The updated recommendations have eliminated the need for routine chest x-rays as all patients now undergo computed tomography. Additionally, “we eliminated the need for the dreaded bone marrow biopsy in patients with Hodgkin lymphoma and most patients with diffuse large B-cell lymphoma because the PET scan will be a better predictor of bone marrow involvement than a simple random bone marrow biopsy. The bone marrow biopsy is a vestige of the past—patients came in and we did things reflexively, we staged them with a bone marrow biopsy,” but PET now provides the same information much less invasively.
Staging terminology has been streamlined by eliminating use of the terms A and B for non-Hodgkin lymphoma and use of X to denote bulky disease, and by recommending a switch from the 1, 2, 3, and 4 numerical staging system (the Ann Arbor classification) to a simple dichotomous one of limited disease and advanced disease, reflecting how hematologists have typically grouped patients for treatment in real-world practice.
Response Assessment Recommendations
For assessing treatment response, the recommendations endorse use of the 5-point Deauville scale that has been internationally validated as a means of standardization. “The scale has been coming into use slowly but has not been widely recognized because people have not been informed about it,” Dr. Cheson commented. “Now it’s going to be the way for the foreseeable future to interpret PET scans so that how one person interprets the scan will be more likely the way another person does. There used to be considerable interobserver or interinterpreter variability.”
The recommendations also outline new definitions of complete response, partial response, and progressive disease. In particular, “a patient can get a complete response in the presence of a mass as long as the mass is no longer avid, and progressive disease can now be determined on the basis of a single node,” he noted.
Finally, “we also made recommendations on management of patients posttreatment, how best to follow patients, where imaging fits in, where it doesn’t fit in, and those sorts of issues,” Dr. Cheson said. ■
Disclosure: Dr. Cheson has served in a consultant or advisory role for Gilead, Celgene, Genentech, Pharmacyclics, AstraZeneca, and Spectrum. He has received honoraria from Gilead, Celgene, Genentech, and Pharmacyclics, and other remuneration from Gilead, Celgene, Genentech, and Pharmacyclics. For full disclosure of all study authors, visit JCO.org.
References
1. Cheson BD, Fisher RI, Barrington SF, et al: Recommendations for initial evaluation, staging and response assessment of Hodgkin and non-Hodgkin lymphoma—the Lugano Classification. J Clin Oncol. August 11, 2014 (early release online).
2. Cheson BD, Pfistner B, Juweid ME, et al: Revised response criteria for malignant lymphoma. J Clin Oncol 25:579-586, 2007.