Using a CA-125 blood test combined with transvaginal ultrasound for early detection of ovarian cancer failed to reduce the risk of mortality associated with the disease and led to a large number of false-positive tests with unnecessary related biopsies and other follow-up procedures in the large, long-term Prostate, Lung, Colorectal, and Ovarian (PLCO) Screening Trial sponsored by the NCI.
The authors said that although CA-125 and transvaginal ultrasound are appropriate for widespread use to evaluate symptoms, assess disease status, and determine the effectiveness of treatments in women already diagnosed with the disease, this study shows that the tests are not useful for general screening in women without the disease. They presented their findings at the ASCO Annual Meeting.1
Precise Screening Tools Needed
 “In the absence of a good method for diagnosing ovarian cancer, we hypothesized that these two tests—which are useful to measure disease—would identify ovarian cancer at an early stage when it is more likely to be cured,” stated lead author Saundra S. Buys, MD, Professor of Medicine at the University of Utah and Huntsman Cancer Institute in Salt Lake City. She said the results were disappointing, “but not necessarily surprising.” Also, Dr. Buys continued, “they show that the tests can actually cause harm, due to the high number of false-positives necessitating surgical biopsies and other related procedures. These results underscore the need for a continuing search to find precise screening tools for the early identification of ovarian cancer.”
“In the absence of a good method for diagnosing ovarian cancer, we hypothesized that these two tests—which are useful to measure disease—would identify ovarian cancer at an early stage when it is more likely to be cured,” stated lead author Saundra S. Buys, MD, Professor of Medicine at the University of Utah and Huntsman Cancer Institute in Salt Lake City. She said the results were disappointing, “but not necessarily surprising.” Also, Dr. Buys continued, “they show that the tests can actually cause harm, due to the high number of false-positives necessitating surgical biopsies and other related procedures. These results underscore the need for a continuing search to find precise screening tools for the early identification of ovarian cancer.”
Study Design and Results
The randomized multicenter study included 78,216 women aged 55 to 74 years screened at 10 screening centers across the United States. They were randomly assigned in a 1:1 ratio to annual screening (CA-125 testing for 6 years, transvaginal ultrasound for 4 years, and follow-up for 13 years) or usual care (no annual screening tests) between 1993 and 2001.
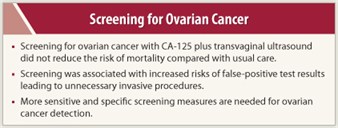 No statistically significant difference was found between the two arms for ovarian cancer cases or related mortality. Ovarian cancer was diagnosed in 212 women in the screening arm compared with 176 in the usual care arm. 118 deaths were reported in the screening arm and 100 in the usual care arm. A total of 2,924 and 2,914 deaths from causes other than ovarian, colorectal, and lung cancer occurred in the two arms, respectively.
No statistically significant difference was found between the two arms for ovarian cancer cases or related mortality. Ovarian cancer was diagnosed in 212 women in the screening arm compared with 176 in the usual care arm. 118 deaths were reported in the screening arm and 100 in the usual care arm. A total of 2,924 and 2,914 deaths from causes other than ovarian, colorectal, and lung cancer occurred in the two arms, respectively.
In the screening arm, there were 3,285 false-positive tests compared with 212 true-positives. About one-third of the women with false-positive tests (n = 1,080) had surgical biopsy; serious complications were reported in 163 of these women. ■
Disclosure: Dr Buys reported no potential conflicts of interest.
Expert Point of View: Screening for Ovarian Cancer Does Not Reduce Mortality and Leads to Unnecessary Tests for False-Positives
Reference
1. Buys SS, Partridge E, Black A, et al: Effect of screening on ovarian cancer mortality in the prostate, lung, colorectal, and ovarian (PLCO) cancer randomized screening trial. 2011 ASCO Annual Meeting. Abstract 5001. Presented June 4, 2011.

