Guest Editor’s Note: Advances in cancer treatments have led to an increase in survival rates, but the quality of life is often diminished during survivorship. Because modifiable personal behavior contributes to health-care outcomes, interventions that support healthy behaviors may improve health while decreasing health-care costs, even in oncology care. In this article, Drs. McManamon, López, and Jonas summarize the approaches intended to facilitate the delivery of whole-person cancer care in a systematic way.

Alyssa McManamon, MD, FACP

Ana María López, MD, MPH, MACP, FRCP, FASCO

Wayne B. Jonas, MD
In oncology, health-care teams focus on treating cancer while caring for the person with cancer. However, our patients often feel they are lost in this process,1 as the bulk of time spent in clinical interaction is focused on disease management. Yet we know that the growing number of cancer survivors want to live as well as possible for as long as possible. Given rising health-care costs, an increased understanding of the impact of social determinants on health and the acknowledgment that medical care contributes to only 11% of health outcomes, many of us are seeking a better approach to health care. Recognizing that modifiable personal behavior contributes to more than one-third of health-care outcomes,2 interventions that support healthy behaviors may improve health while decreasing health-care costs—even in cancer care.
What Constitutes Whole-Person Health?
The U.S. Department of Veterans Affairs (VA) has rolled out a Whole Health System that “supports person-centered, proactive, whole-person care. This System includes conventional treatment, complementary and integrative health approaches, and focuses on self-empowerment, self-healing, and self-care.”3
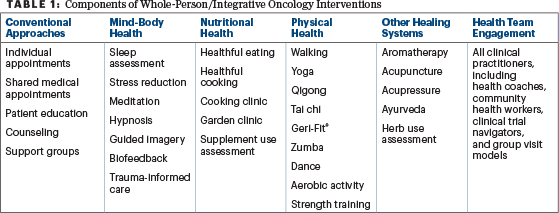
Whole Health is described as an approach that shifts the clinical focus from “What’s the matter with you?” to “What matters to you?” This shift engages clinical care beyond the traditional individual disease-alone–focused appointment (see Table 1) and incorporates community building through group experiences.
The National Academies of Sciences, Engineering, and Medicine recently published “Achieving Whole Health: A New Approach for Veterans and the Nation.”4 The study notes that this approach is promising and transformative. Whole health is delineated as “…physical, behavioral, spiritual, and socioeconomic well-being as defined by individuals, families, and communities.” The foundational elements of whole person care are outlined as people-centered, comprehensive and holistic, upstream-focused, accountable and equitable, and grounded in team well-being.
Guest Editor

Jun J. Mao, MD, MSCE
Building on work in primary care,5 a 13-institution, 2-year leadership collaborative came together in 2021 to further improve whole-person care in oncology. Sponsored by the Samueli Foundation and Healing Works Foundation, the collaborative included both academic and community-based oncology practices in the United States and abroad. The collaborative engaged integrative oncologists and other health professionals skilled in whole-person and evidence-informed care that integrates healing systems into mainstream practices.
The collaborative developed freely available and actionable cancer care6 tools and resources intended to facilitate the delivery of whole-person care in a systematic and routine way. All resources are available for single-institution rebranding, under Creative Commons, and can be found on the Healing Works Foundation website at https://healingworksfoundation.org.
Steps Toward Whole-Person Cancer Care
Here are several steps to take to begin the process toward whole-person cancer care:
- Edit your intake process to invite a whole-person discussion and document it in the electronic health record. The Personal Health Inventory (PHI) is a brief intake form adapted from the VA and piloted for use by various institutions, with a version specifically tailored for cancer care. The PHI puts “what matters” for the person into the center of discussion, along with areas of health amenable to self-management or further referrals. By creating discourse, the PHI and supporting resources help uncover the social determinants that matter to the person earlier, which allows the health-care team to address needs better.
- Review the guidelines. The National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology (NCCN Guidelines®) include behavioral, nonpharmaceutical, and non-Western medicine recommendations. Similarly, the recent Society for Integrative Oncology (SIO)-ASCO Guidelines on anxiety and depression and cancer pain management7,8 include such recommendations as well. Recent advances in cancer biology reveal the impact of behavioral change on the tumor macro- and microenvironments, on the interplay of immunotherapy with microbiome function, and on the effect of physical activity on cancer outcomes.
- Innovate and learn more about whole-person care.9 More than two-thirds of oncologists say they want to learn more about whole-person and integrative oncology approaches.10 Accessible pocket guides on the evidence related to healing practices such as acupuncture and guided imagery are freely available. Look for educational opportunities and fellowships in integrative medicine and/or oncology. A guidebook on whole-person cancer care for health-care teams, Healing and Cancer (coauthored by WBJ and AM) and a no-cost continuing medical education course from Tufts University are now available, along with a related podcast How Healing Works (Season 2). There are also resources available to learn how your team can offer group medical visits11 to hasten recovery, improve efficiency, and create community for the people you serve.
- Uplevel your self-care. Explore a healing modality for yourself. When it comes to whole-person care, learning through self-application can be significant and may help to guide your patients better. Fill out your own PHI and see what you discover. Try it as a team.
A Call to Action
We invite you to join the transformation and think about whole-person cancer care by flagging a few precious minutes at the first visit to affirm to patients that their wholeness matters. You may open the conversation on how behavior and lifestyle enhance quality and quantity of life for persons with cancer. You may drive process improvement toward whole-person care. You may allow yourself to care better for yourself. As we permit ourselves these acts of transformation, we embrace our inherent kindness12 and may lessen the fear in cancer care, provide better care for the person with cancer, and begin to innovate from a new and different perspective from which new and better results may emerge.
DISCLOSURE: Dr. McManamon, Dr. López, and Dr. Jonas reported no conflicts of interest.
REFERENCES
1. Institute of Medicine and National Research Council: From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC; National Academies Press; 2006.
2. Goinvo: Determinants of Health. Available at https://www.goinvo.com/vision/determinants-of-health. Accessed August 22, 2024.
3. U.S. Department of Veterans Affairs: Whole Health: Integrative Health & Wellness. Available at https://www.va.gov/madison-health-care/health-services/whole-health. Accessed August 22, 2024.
4. National Academies of Sciences, Engineering, and Medicine: Achieving Whole Health: A New Approach for Veterans and the Nation. Washington, DC; National Academies Press; 2023.
5. Rosenbaum E, Gordon AE, Cresta J, et al: Implementing whole person primary care: Results from a year-long learning collaborative. J Am Board Fam Med 36:542-549, 2023.
6. Jonas WB, McManamon A, Lerner M, et al: New tools for bringing whole person care into routine oncology, 2023 Society for Integrative Oncology Conference. Abstract 19. Presented September 15, 2023.
7. Carlson LE, Ismaila N, Addington EL, et al: Integrative oncology care of symptoms of anxiety and depression in adults with cancer: SIO-ASCO guideline summary and Q&A. JCO Oncol Pract 19:847-851, 2023.
8. Mao JJ, Greenlee H, Bao T, et al: Integrative medicine for pain management in oncology: Society for Integrative Oncology–ASCO guideline summary and Q&A. JCO Oncol Pract 19:45-48, 2023.
9. Dearing JW, Cox JG: Diffusion of innovations: Theory, principles, and practice. Health Aff (Millwood) 37:183-190, 2018.
10. Patients with cancer may be interested in complementary therapies, survey says. The ASCO Post, October 13, 2023.
11. Thompson-Lastad A, Atreya CE, Chao MT, et al: Improving access to integrative oncology through group medical visits: A pilot implementation project. J Altern Complement Med 25:733-739, 2019.
12. Berry LL, Danaher TS, Chapman RA, et al: Role of kindness in cancer care. J Oncol Pract 13:744-750, 2017.
Dr. McManamon is Associate Professor of Medicine at Boonshoft School of Medicine–Wright State University and is a clinical faculty member of Dayton VA Medical Center. Dr. López is Professor and Vice Chair, Medical Oncology, Sidney Kimmel Medical College; Medical Director, Medical Oncology and Chief of Cancer Services, Jefferson Health New Jersey, Sidney Kimmel Cancer Center; and President-Emeritus of the American College of Physicians. Dr. Jonas is President of the Healing Works Foundation and Clinical Professor at Georgetown University School of Medicine, Uniformed Services University of the Health Sciences.
Disclaimer: The views, opinions, conclusions, or recommendations expressed in this article belong solely to the authors and do not necessarily state or reflect the views of any organization or agency or those of the U.S. government.

