The Society for Integrative Oncology (SIO) and ASCO have released a guideline that appraises the evidence to support incorporating integrative medicine approaches into managing pain in adults with cancer.1 The guideline builds upon existing ASCO guidelines on pain management, the growing body of research in this area, and emphasis from the Centers for Disease Control and Prevention to utilize nonpharmacologic approaches for pain management.2-4
The guideline is an effort to synthesize evidence-based data informed by randomized clinical trials and systematic reviews guided by clinical experience. A multidisciplinary group of experts developed the recommendations contained in the guideline. A total of 227 articles in the literature, published between 1990 and 2021, formed the evidentiary basis for the guideline recommendations. The trials compared various integrative therapies with the standard of care, placebos, sham interventions, other interventions, or active controls.
Guideline Rationale
“Many oncologists and oncology [health-care providers] struggle with managing pain adequately for patients with cancer using conventional pain approaches, particularly with the ongoing opioid epidemic, and certainly many patients also desire to use methods in addition to conventional pain management,” said Jun J. Mao, MD, MSCE, of Memorial Sloan Kettering Cancer Center, and SIO Co-Chair of the guideline expert panel, in explaining the rationale for the guideline.
“We know that up to 79% of patients with cancer seek some level of integrative interventions to help them cope with their cancer but also to help them feel better and improve their quality of life,”5-7 said Eduardo Bruera, MD, of The University of Texas MD Anderson Cancer Center, and ASCO Co-Chair of the guideline expert panel. “Pain is clearly one of the most difficult situations for a patient with cancer, particularly advanced cancer, but also for cancer survivors, who have completed their treatment and have chronic pain related to some of the treatments they received. They seek ways to help themselves in addition to the traditional treatments offered by their physicians.”
Integrative medicine has not received the same level of attention from industry or the level of funding from grantors compared with more traditional oncology interventions, hence the evidence to support integrative approaches is more limited than that for the conventional interventions. “Although the interventions themselves are not expensive, the process of conducting the research can be expensive, which can create a barrier to generating evidence,” he said.
Understanding the Evidence Behind Integrative Medicine
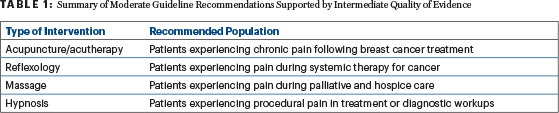
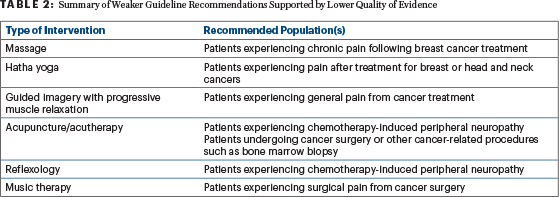
Dr. Bruera said the purpose of the guideline is to help busy medical oncologists understand the evidence behind integrative medicine interventions, so they can engage in a candid discussion with patients who may be interested in incorporating them into their pain management regimen. Tables 1 and 2 summarize key recommendations from the guideline, separated by the strength of the recommendation and the quality of evidence supporting the guidance.
In all cases, the benefits of each type of intervention were considered to outweigh the potential harms. The use of other integrative medicine interventions for other types of pain currently has lower quality of evidence, according to the panel.
Many of the National Cancer Institute–designated comprehensive cancer centers already offer some integrative therapies, such as acupuncture and massage. “However, most patients with cancer are treated in community oncology settings. We hope clinical guidelines like this will increase the uptake of these therapies, in addition to conventional pain management, to help patients with cancer manage their symptoms and to improve their quality of life and function,” Dr. Mao said. “Furthermore, we hope the ASCO and clinical guidelines can stimulate a policy change, so some of these treatments can be covered by insurance to increase access further and address disparities in pain management.”
Dr. Bruera said he hopes the publication of the guideline will spur an interest in further research into the potentially effective interventions mentioned. “Perhaps readers will want to move into conducting studies with a stronger methodological design and test an integrative intervention with an open mind and an equipoised approach to determine if an intervention will work better than another control intervention in a particular patient population,” he said.
REFERENCES
1. Mao JJ, et al: J Clin Oncol. September 19, 2022 (early release online).
2. Paice JA, et al: J Clin Oncol 34:3325-3345, 2016.
3. Loprinzi CL, et al: J Clin Oncol 38:3325-3348, 2020.
4. Dowell D, et al: MMWR Recomm Rep 65:1-49, 2016.
5. Mao JJ, et al: Complement Ther Med 15:21-29, 2007.
6. Mao JJ, et al: J Cancer Surviv 5:8-17, 2011.
7. John GM, et al: J Cancer Surviv 10:850-864, 2016.
Originally published in ASCO Daily News. © American Society of Clinical Oncology. ASCO Daily News, September 21, 2022. All rights reserved.

