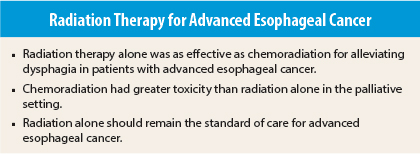
Radiation therapy alone was found to be as effective as chemoradiation in reducing dysphagia associated with advanced esophageal cancer in the palliative setting and was less toxic, according to results of a multinational phase III trial called the Trans-Tasman Radiation Oncology Group (TROG) 03.01 and National Cancer Institute of Canada (NCIC) CTG ES.2. Results of the study were presented at the 56th Annual Meeting of the American Society for Radiation Oncology (ASTRO).1
Radiation an Excellent Tool in Palliation
“Overall, radiation remains an excellent tool for palliation of patients with advanced esophageal cancer and should remain the standard of care,” said lead author Michael Gordon Penniment, MBBS, Director of Radiation Oncology at Royal Adelaide Hospital in South Australia and the Director of Radiation Oncology at the Alan Walker Cancer Chemotherapy Care Centre in Darwin, Australia.
Researchers found that chemotherapy increased toxicity significantly without additional symptom control or improved survival in this patient population. “The study focused on the best, yet simplest and least toxic treatment to alleviate pain,” Dr. Penniment said.
“There is no gold standard for palliation [in this setting]. Current practice is to prescribe chemotherapy for patients with advanced esophageal cancer, presumably based on the standard use of [chemoradiotherapy] in patients with less advanced disease,” Dr. Penniment said. “These results will allow us to simplify treatment for patients [whose disease is incurable] but who can expect an improvement in swallowing and quality of life with radiation alone, sparing them the extra toxicity and cost of chemotherapy.”
Study Details
This is the largest randomized phase III trial in advanced esophageal cancer. The study enrolled 220 patients, the majority with metastatic disease, and randomized them to receive palliative radiation (35 Gy in 15 fractions in Australia and New Zealand or 30 Gy in 10 fractions in Canada and the United Kingdom) or concomitant chemoradiotherapy with cisplatin and fluorouracil. Dysphagia was measured with the Mellow score; toxicity with the Common Terminology Criteria for Adverse Events (CTCAE) version 2, and quality of life (QOL) using the European Organization for Research and Treatment of Cancer (EORTC) QLQ 30 and esophagus module (OES-18).
Results
A dysphagia response at any time was reported in 67.89% of patients in the radiotherapy-alone group vs 73.8% in the chemoradiotherapy group, a difference that was not statistically significant. However, chemoradiotherapy resulted in a significant increase in toxicity, namely, nausea and vomiting (P < .01), compared with radiotherapy alone. Median survival was not significantly different between the two treatment arms.
One potentially important finding of the trial was that about 10% (n = 21) of patients were alive 2 years post-treatment. “This tail in the curve shows us that there is a small group of patients with primary advanced esophageal cancer who can have longer-term survival, and radiation can improve swallowing and potentially lengthen the time without symptoms in this group,” Dr. Penniment said.
“We think all patients with esophageal cancer can potentially benefit from radiation,” he said. ■
Disclosure: Dr. Penniment reported no potential conflicts of interest.
Reference
1. Penniment MG, Harvey JA, Wong R, et al: Best practice in advanced oesophageal cancer: A report on TROG 03.01 NCIC CTG ES.2 multinational phase III study in advanced oesophageal cancer comparing quality of life and palliation of dysphagia in patients treated with radiotherapy or chemo-radiotherapy. ASTRO Annual Meeting. Abstract CT-03. Presented September 14, 2014.