Researchers at the Salk Institute have reported on a synthetic derivative of vitamin D able to collapse the barrier of cells shielding pancreatic tumors, making this challenging cancer more susceptible to therapeutic drugs. The discovery has led to human trials for pancreatic cancer, even in advance of the publication of the study recently in Cell.1
These findings may also have implications for other difficult-to-treat tumors, such as lung, kidney, and liver cancer.
“While the success of this drug in humans with pancreatic cancer is still unclear, the findings in animal studies were strong, raising hope that ongoing clinical trials will give people with this terrible disease hope for a truly new type of therapy,” said Ronald M. Evans, PhD, Director of Salk’s Gene Expression Laboratory and Senior Author of the recent paper.
Resistance to Therapy An Ongoing Challenge
“For pancreatic cancer, the 5-year survival rate is the lowest of all cancers,” said Dr. Evans, Holder of Salk’s March of Dimes Chair and a Howard Hughes Medical Institute Investigator. “Part of the problem is that the science of pancreatic cancer and its renowned resistance to therapy has not been understood and that’s why the work that we’re doing is so important.”
Dr. Evans and his colleagues knew that the ability of the pancreatic tumor to communicate with the tumor microenvironment was key to its growth. This “living shield” around a tumor not only helps the cancer grow, but blocks the access of immune cells and chemotherapeutic drugs, making the cancer particularly hard to treat.
Exploring the Tumor Microenvironment
In collaboration with researchers around the country involved in an interdisciplinary initiative supported by Stand Up to Cancer, Dr. Evans wanted to determine how to restore the tumor microenvironment to its normal state and weaken the wall around the tumor.
“There was evidence that the activation of the microenvironment was theoretically reversible, but nobody knew exactly what was responsible for the activation, making it hard to turn off,” said Mara Sherman, PhD, a Salk Postdoctoral Research Fellow and first author.
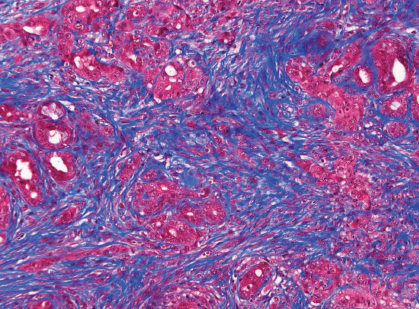
Drs. Sherman, Evans, and their collaborators focused their attention on one component of this wall: pancreatic stellate cells, which usually respond to small injuries by briefly switching to an activated state, spurring new cell growth. In the case of cancer, however, the stellate cells near a tumor are constantly turned on in response to signals from the tumor. This chronic activation of the stellate cells provides the tumor cells with extra growth factors and therefore helps them proliferate, but also forms a wall-like barrier around the tumor that protects it from chemotherapeutics and other anticancer drugs.
In 2013, Evans’ group discovered that stellate cells in the liver could be inactivated by a chemically modified form of vitamin D. They wondered whether the same could hold true in the pancreas, despite the fact the vitamin D receptor was not thought to be present in pancreatic tissue.
When the group of researchers examined the differences between activated and inactivated stellate cells in the pancreas, they found that activated stellate cells near a tumor had high levels of the vitamin D receptor. And when the researchers then added modified vitamin D to activated stellate cells the cells quickly reverted back to a healthy, inactivated state, stopping production of signals that spur growth and inflammation.
“This was a big surprise because vitamin D has been tried multiple times as a therapy for pancreatic cancer and never worked,” said Dr. Evans. It turned out that activated stellate cells rapidly break down normal vitamin D, preventing the vitamin from binding to the receptor, Dr. Evans explained. But systematic analysis of vitamin D analogues allowed the team to discover a modified form of vitamin D that is more stable, resilient, and effective in vitro.
Novel Vitamin D–Like Compound
To see whether this new vitamin D–like compound could halt the growth of a tumor, Dr. Evans and his team next studied its effectiveness in mice. The researchers found that combining the drug with existing chemotherapeutics gave a 50% increase in life span compared to chemotherapy alone.
“It’s really remarkable considering that vitamin D itself is not attacking the cancer cells,” said Michael Downes, PhD, a senior staff scientist at Salk and co–corresponding author of the new work. “It’s changing the environment to a more favorable setting needed for the chemotherapy drugs to work.”
Studies have shown that people deficient in vitamin D are more likely to develop pancreatic cancer. Based on the new results, Dr. Evans thinks that healthy levels of vitamin D may help keep vitamin D receptor signaling in stellate cells normal and squash a cancer’s growth, at least until a tumor itself forces the stellate cells to “turn on.”
“Recently, other research groups have explored the idea of destroying the microenvironment altogether to weaken a tumor,” said Dr. Downes. “Our approach is very different. Instead of destroying, we simply want to reprogram the tumor microenvironment to a healthy state. This has the dual effects of delivering more drugs to the tumor as well as replenishing the tissue with normal stellate cells.”
Next Steps
Dr. Evans’ group has teamed up with clinicians at the University of Pennsylvania to launch a clinical trial testing the effectiveness of using their vitamin D–like drug in cancer patients before pancreatic surgery.
“Previous trials with vitamin D failed because they didn’t understand the need for a special form of vitamin D and that for pancreatic cancer it must be used in combination with chemotoxic drugs,” Dr. Evans said. “So, by rethinking the problem, we have been able to open up a new route to the treatment of pancreatic cancer and, looking forward, hopefully other diseases as well.” ■
Reference
1. Sherman MH, Yu RT, Ding N, et al: Vitamin D receptor-mediated stromal reprogramming suppresses pancreatitis and enhanses pancreatic cancer therapy. Cell 159:80-93, 2014.