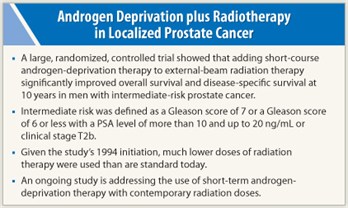
The addition of short-term androgen-deprivation therapy to external-beam radiation therapy improved overall and disease-specific survival in men with nonbulky localized prostate cancer and prostate-specific antigen (PSA) levels up to 20 ng/mL, as reported recently in The New England Journal of Medicine.1 The benefit of the addition of short-term  androgen-deprivation therapy was seen mainly in men with intermediate-risk disease, not low-risk disease, in this large, randomized, phase III international trial.
androgen-deprivation therapy was seen mainly in men with intermediate-risk disease, not low-risk disease, in this large, randomized, phase III international trial.
A caveat about these findings is that the radiation techniques used in this study were those used in 1994, when the study was initiated. More sophisticated techniques now in use deliver higher doses than what was possible 17 years ago. The benefit of short-term androgen-deprivation therapy has not been proven with the newer techniques, said lead author Christopher Jones, MD, a radiation oncologist at Radiological Associates in Sacramento, California.
Current Practice
Currently, most patients receive intensity-modulated radiation therapy, and many opt for treatment with brachytherapy (delivered via seeds [low-dose] or catheter [high-dose]). These newer techniques are associated with improved efficacy, Dr. Jones noted, which raises the question of the value of short-term androgen-deprivation therapy when added to modern radiotherapy techniques in intermediate-risk prostate cancer.
“It is not correct to routinely give short-term androgen-deprivation therapy to all patients on high doses of radiation delivered by modern techniques,” Dr. Jones stated.
The ongoing Radiation Therapy Oncology Group (RTOG) 0815 study is designed to answer the question of whether short-term androgen-deprivation therapy should be given with high-dose radiation, he explained. That study is currently accruing over 1,500 intermediate-risk patients who will be randomly assigned to high-dose radiation (physician’s choice of technique) with or without short-term androgen-deprivation therapy (6 months in the new study).
NEJM Study Details
 The study by Jones and colleagues (RTOG 94-08) enrolled 2,028 patients from 212 centers in the United States and Canada with localized prostate cancer (stages T1b, T1c, T2a, or T2b) and PSA levels ≤ 20 ng/mL. About 48% of cancers were T1, and about 52% were T2. About 63% had Gleason score 2 to 6, about 28% were Gleason 7, and about 9% were Gleason 8 to 10; a small percentage—about 2%—had unknown Gleason scores. Participants received no previous treatment for prostate cancer and were randomized to receive short-term androgen-deprivation therapy (2 months before radiotherapy and 2 months during radiotherapy) plus radiotherapy or radiotherapy alone. A total radiation dose of 66 Gy was delivered to the pelvis and prostate.
The study by Jones and colleagues (RTOG 94-08) enrolled 2,028 patients from 212 centers in the United States and Canada with localized prostate cancer (stages T1b, T1c, T2a, or T2b) and PSA levels ≤ 20 ng/mL. About 48% of cancers were T1, and about 52% were T2. About 63% had Gleason score 2 to 6, about 28% were Gleason 7, and about 9% were Gleason 8 to 10; a small percentage—about 2%—had unknown Gleason scores. Participants received no previous treatment for prostate cancer and were randomized to receive short-term androgen-deprivation therapy (2 months before radiotherapy and 2 months during radiotherapy) plus radiotherapy or radiotherapy alone. A total radiation dose of 66 Gy was delivered to the pelvis and prostate.
The addition of short-term androgen-deprivation therapy led to a modest but significant improvement in overall survival at 10 years, from 57% with radiotherapy alone to 62% with short-term androgen-deprivation therapy (P = .03). Ten-year disease-specific mortality was also reduced, from 8% to 4% (P = .001), along with a reduction in the secondary endpoints of biochemical failure (as shown by PSA level), distant metastases, and positive biopsy rate at 2 years.
In a multivariate analysis, a Gleason score of 7 or higher was a negative predictive factor for overall survival, disease-free survival, distant metastases, and biochemical failure. Other negative prognostic factors were older age and nonwhite race for overall survival; clinical T2 lesions for disease-specific mortality; and PSA ≥ 4 ng/mL for biochemical failure.
Subgroup Analysis
When the data were reanalyzed according to subgroups, the gains in overall survival and disease-free survival with short-term androgen-deprivation therapy were limited mainly to men in the intermediate-risk group (intermediate risk was defined as a Gleason score of 7 or a Gleason score of 6 or less with a PSA level of more than 10 and up to 20 ng/mL or clinical stage T2b). The 10-year overall survival rate was increased from 54% to 61%, and 10-year disease-specific mortality was reduced from 10% to 3% with the addition of short-term androgen-deprivation therapy in intermediate-risk men.
The benefits of short-term androgen-deprivation therapy were achieved with minimal toxic effects, including serious cardiovascular effects and long-term gastrointestinal or genitourinary complications of radiotherapy. The addition of short-term androgen-deprivation therapy had a somewhat stronger impact on erectile function than radiotherapy alone; responses on a Sexual Adjustment Questionnaire showed that although 73% of androgen-deprivation therapy group were able to have erections always, almost always, or sometimes pretreatment, only 44% had this response at 1 year. In the radiotherapy-alone group, 79% reported good pretreatment erectile function compared with 54% at 1 year. ■
Disclosure: Dr. Jones reported no potential conflicts of interest.
Expert Point of View: Short-term Androgen Deprivation plus Radiotherapy Improves Outcomes in Intermediate-risk Prostate Cancer
Reference
1. Jones C, Hunt D, McGowan DG, et al: Radiotherapy and short-term androgen deprivation for localized prostate cancer. N Engl J Med 365:107-118, 2011.

