 At the Best of ASCO Miami meeting, Daniela Matei, MD, Indiana University Melvin and Bren Simon Cancer Center, Indianapolis, described how new approaches are significantly prolonging remission in ovarian cancer.
At the Best of ASCO Miami meeting, Daniela Matei, MD, Indiana University Melvin and Bren Simon Cancer Center, Indianapolis, described how new approaches are significantly prolonging remission in ovarian cancer.
Ovarian Screening Provides No Benefit
The Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial, which employed annual simultaneous CA-125 and transvaginal ultrasound over 4 to 6 years, did not reduce ovarian cancer mortality, and there was, in fact, evidence of harm from diagnostic evaluations and surgery following false-positive screens.1 The randomized study involved 78,216 women aged 55 to 74, enrolled between 1993 and 2001 and followed until February 2010.
At a median follow-up of 12.4 years, cancer was identified in 212 women in the intervention arm and 176 under usual care, while ovarian cancer deaths were recorded in 118 and 100, respectively. Stage I/II tumors were found in 47 and 38 women, and stage III/IV in 163 and 137, respectively. At 10 years, overall survival was approximately 25% in both arms (P = .18). There were 3,285 false-positive screens, leading to 1,080 surgeries and 222 major complications in 163 patients, including infections in 40% and direct surgical complications in 28%. The oophorectomy rate was 33% higher with the intervention: 7.7% vs 5.8%.
“Screening did not impact the detection of early tumors that could improve survival,” she said, calling the PLCO trial “an important study but with limitations.”
Dr. Matei’s concerns included the variable duration of follow-up from the time of enrollment, the use of fixed CA-125 cutoffs (ignoring individual variation), and the lack of a standardized approach to positive screens. But the trial is consistent with other large studies, she said, which have also found no mortality benefit with screening. Results from the UKCTOCS study in the United Kingdom, expected in 2015, should help determine definitively the value of screening for ovarian cancer.
Maintenance PARP Inhibitor Extends Remission
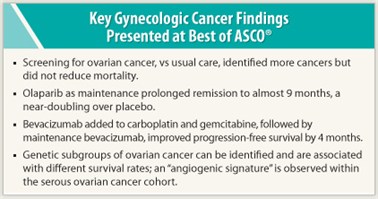 Disease remission was significantly prolonged by maintenance treatment with the poly (ADP-ribose) polymerase (PARP) inhibitor olaparib in the phase II trial of 265 patients with a prior response to platinum regimens.2 Maintenance with olaparib reduced progressive disease by 65%, with median progression-free survival being 8.4 months with olaparib vs 4.8 months with placebo (P < .00001). Disease progressed in 44% (olaparib) and 72% (placebo). Overall survival data are not yet mature.
Disease remission was significantly prolonged by maintenance treatment with the poly (ADP-ribose) polymerase (PARP) inhibitor olaparib in the phase II trial of 265 patients with a prior response to platinum regimens.2 Maintenance with olaparib reduced progressive disease by 65%, with median progression-free survival being 8.4 months with olaparib vs 4.8 months with placebo (P < .00001). Disease progressed in 44% (olaparib) and 72% (placebo). Overall survival data are not yet mature.
Olaparib was well tolerated, though it was associated with increases in nausea (68% vs 35%), fatigue (49% vs 38%), and vomiting (32% vs 14%).
“This is a very timely and important trial,” Dr. Matei commented. An integrated analysis of 500 serous ovarian adenocarcinomas from The Cancer Genome Atlas project found homologous recombination to be defective in 53% of tumors, suggesting that ovarian cancer is a good target not only for platinum agents but also for PARP inhibitors.
Phase III trials of PARP inhibitors in recurrent disease are planned, including an upfront combination of a PARP inhibitor, chemotherapy, and bevacizumab (Avastin) by the Gynecologic Oncology Group. Research efforts should also aim to determine the optimal timing and sequence of such agents, identify predictive biomarkers for homologous repair deficiency, and understand mechanisms of resistance to PARP inhibitors, she said.
Addition of Bevacizumab Extends Remission by 4 Months
Maintenance therapy with bevacizumab also prolonged remission by 4 months in 480 platinum-sensitive patients with recurrent cancer (of the ovaries, peritoneum, or fallopian tubes) in the OCEANS trial.3 Bevacizumab added to carboplatin and gemcitabine, followed by bevacizumab until progression, improved progression-free survival to 12.4 months, from 8.4 with chemotherapy alone—a 52% reduction in risk (P < .0001). Interim overall survival analysis showed a trend toward benefit, with median overall survivals of 35.5 months and 29.9 months, respectively (P = .094).
“Bevacizumab’s activity in ovarian cancer is much higher than in colon, lung, and breast cancers, and comparable to activity in renal cell carcinoma,” Dr. Matei commented. “Three randomized trials have been positive in the adjuvant and recurrent settings. The most benefit has been seen in higher-risk groups—those with recurrent disease and those suboptimally debulked in the adjuvant setting.”
Future studies in ovarian cancer will be needed to answer questions about dose, duration, and patient selection.
‘Angiogenic Signature’ May Select Patients for Bevacizumab
The ideal of establishing molecular profiles to help guide treatment is a step closer, as investigators have identified molecular subgroups using DNA microarray expression data.4 Analysis of formalin-fixed paraffin embedded (FFPE) specimens was linked to prospectively collected clinical data, and six molecularly distinct subgroups were significantly related to histology and to differing overall survival rates (P < .0001). Within the serous cohort, the dominant discriminatory biology was associated with angiogenic processes.
“Expression profiling on macrodissected FFPE specimens is feasible with this novel platform, and the molecular profiling correlates tightly with histologic subtype,” Dr. Matei noted. Pending validation, the 25-gene signature with functional angiogenic significance, ie, “angiogenic signature,” may someday help select patients for bevacizumab. While “we are not there yet” with regard to the molecular classification of ovarian cancer, progress is steady. ■
Disclosure: Dr. Matei has received consulting fees from Genentech.
SIDEBAR: Can Society Afford Bevacizumab in Ovarian Cancer?
References
1. Buys SS, Partridge E, Black A, et al: Effect of screening on ovarian cancer mortality in the Prostate, Lung, Colorectal and Ovarian cancer randomized screening trial. 2011 ASCO Annual Meeting. Abstract 5001. Presented June 4, 2011.
2. Ledermann JA, Harter P, Gourley C, et al: Phase II randomized placebo-controlled study of olaparib (AZD2281) in patients with platinum-sensitive relapsed serous ovarian cancer. 2011 ASCO Annual Meeting. Abstract 5003. Presented June 4, 2011.
3. Aghajanian C, Finkler NJ, Rutherford T, et al: OCEANS: A randomized, double-blinded, placebo-controlled phase III trial of chemotherapy with or without bevacizumab in patients with platinum-sensitive recurrent epithelial ovarian, primary peritoneal, or fallopian tube cancer. 2011 ASCO Annual Meeting. Abstract LBA5007. Presented June 4, 2011.
4. Gourley C, Michie CO, Keating KE, et al: Establishing a molecular taxonomy for epithelial ovarian cancer from 363 formalin-fixed paraffin embedded specimens. 2011 ASCO Annual Meeting. Abstract 5000. Presented June 4, 2011.

