Long-term analysis of the Short-HER trial showed that 9 weeks of adjuvant trastuzumab conveyed benefits comparable to a 1-year course in patients with early HER2-positive breast cancer deemed to be at low or intermediate risk for recurrence. High-risk patients, however, derived considerably more benefit from the conventional longer course, and the study did not meet the noninferiority threshold of significance, investigators reported at the European Society for Medical Oncology (ESMO) Breast Cancer Virtual Congress 2021.1
“Patients classified as being at low or intermediate risk represented 84.6% of the study population. In the follow-up analysis, both disease-free and overall survival curves for those groups were superimposable,” said lead investigator, Pierfranco Conte, MD, of the University of Padua, Italy.

Pierfranco Conte, MD
This study was designed to assess whether a shorter trastuzumab course is noninferior to a conventional 1-year course with respect to disease-free survival. A hazard ratio (HR) less than 1.29 was set as a noninferiority margin.
Although 1 year of adjuvant trastuzumab remains the standard, stated Dr. Conte, “for a large proportion of real-world patients with HER2-positive early breast cancer,” less treatment may be acceptable, but de-escalation strategies should be tested in clinical trials.
About Short-HER
The Short-HER trial randomly assigned 1,254 patients with HER2-positive early breast cancer to receive chemotherapy plus 9 weeks vs 1 year of adjuvant trastuzumab. More than half of patients had node-negative disease and thus were at low risk for recurrence, Dr. Conte noted.
Chemotherapy in the long treatment arm was doxorubicin or epirubicin plus cyclophosphamide for 4 courses, followed by a taxane for 4 courses; trastuzumab was given every 3 weeks for 18 doses. Chemotherapy in the short arm was docetaxel for three courses followed by fluorouracil, epirubicin, and cyclophosphamide for three courses; trastuzumab was given for 9 weeks.
At the previously reported event-driven analysis, which was conducted after a median follow-up of 6 years, disease-free survival rates at an 8-year median follow-up were 88% in the long arm and 85% in the short arm (HR = 1.13; 90% confidence interval [CI] = 0.89–1.42), with the upper limit of the confidence interval crossing the noninferiority margin set at 1.29.2 Thus, noninferiority could not be claimed at that time, he said.
Shorter treatment was associated with less cardiotoxicity. Grade ≥ 2 cardiac adverse events were observed in 4.3% of the short treatment arm and 13.1% of the long treatment arm, yielding a risk ratio of 0.33 favoring the shorter treatment (P < .001).
Long-Term Follow-up
At the ESMO Breast cancer Virtual Congress, Dr. Conte presented the overall survival analysis (the co-primary endpoint of the study) and updated disease-free survival according to hormone receptor status and the three risk categories: low risk (pT < 2 cm and pN0), which was 38% of the population; intermediate risk (pT < 2 cm and 1–3 pN+ or pT > 2 cm and 0–3 pN+), which was 47% of the population; and high risk (any pT and 4+ pN+), which was 15% of the population.
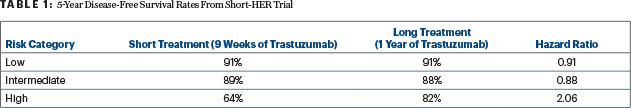
At a median follow up of 8.7 years, disease-free survival events numbered 121 in the short treatment arm and 116 in the long treatment arm (HR = 1.09; 90% CI = 0.88–1.35). The hazard ratios by risk category were comparable between the arms, except for in the high-risk category (Table 1). According to hormone receptor status, hazard ratios were 1.11 for patients with hormone receptor–positive disease and 1.06 for patients with hormone receptor–negative disease. At 9 years, overall survival rates were 90% after 9 weeks of trastuzumab and 91% with 1 year of treatment (HR = 1.18; 90% CI = 0.86–1.62), he reported.
Dr. Conte said that, because outcomes are good with 9 weeks of trastuzumab, a short course could be an option in populations with limited access to trastuzumab and for patients with cardiotoxicity concerns. “Our data are also reassuring for patients who have to discontinue trastuzumab due to a decline in left-ventricular ejection fraction,” he added. “You can safely reassure such patients that they can probably stop treatment without compromising outcomes.”
DISCLOSURE: Dr. Conte has served as a consultant or advisor to Daiichi Sankyo/Lilly; has participated in a speakers bureau for AstraZeneca, Bristol Myers Squibb, Eli Lilly, Novartis, Roche/Genentech, and Tesaro; has received institutional research funding from Bristol Myers Squibb, Merck KGaA, Novartis, and Roche; has provided expert testimony on behalf of AstraZeneca and Roche; and has been reimbursed for travel, accommodations, or other expenses by AstraZeneca, Celgene, Novartis, and Pfizer.
REFERENCES
1. Conte PF, Frassoldati A, Bisagni G, et al: Nine weeks vs 1 year adjuvant trastuzumab: Long-term outcomes of the Short-HER randomised trial. ESMO Breast Cancer Virtual Congress 2021. Abstract 410. Presented May 7, 2021.
2. Conte P, Frassoldati A, Bisagni G, et al: Nine weeks versus 1 year adjuvant trastuzumab in combination with chemotherapy: Final results of the phase III randomized Short-HER study. Ann Oncol 29:2328-2333, 2018.

