In this first installment of our history of geriatric oncology, we outline what we consider the most relevant steps in the prehistory and past history of geriatric oncology. In a future issue of The ASCO Post, we will explore the contemporary history of the field.
The Prehistory of Geriatric Oncology
The prehistory of geriatric oncology coincides with the development of systemic treatments of cancer. The lessons learned during these initial experiences showed that age was a predisposing factor to the development of cancer and, in general, a poor prognostic factor that included increased risk of treatment complications. Those early observations led to the questions that eventually defined the scope of geriatric oncology: Is the poorer prognosis due to a more aggressive disease, to inadequate treatment, or to delayed diagnosis? How can we prevent treatment toxicity in the older person? Most important of all how do we define “old” in functional terms?
Here, we outline what we consider the most relevant steps in the prehistory of geriatric oncology.
Systemic Therapies’ Influence on Geriatric Oncology
Although it might not have been justified in light of our current knowledge about treatment protocol, in the mid-20th century, there was an attempt to adjust treatment for breast cancer based on a patient’s age. The first systemic treatment for breast cancer was hormonal therapy. In the 1950s and 1960s, premenopausal women with metastatic breast cancer were treated with ovarian ablation, whereas postmenopausal women were treated with high-dose estrogens.10a
Acute leukemias were one of the first diseases benefiting from cytotoxic chemotherapy. During the 1960s, the management of acute lymphoblastic leukemia in children appeared promising, whereas patient outcomes became poorer and poorer with advancing age.11 Around the same time, the development of cytarabine allowed the achievement of frequent complete remissions and, in some cases, prolonged survival in younger adults with acute myeloid leukemia (AML).12,13
“The conference on Cancer in the Elderly promoted worldwide interest in geriatric oncology, and the establishment of SIOG provided a worldwide organization focused on geriatric oncology....”— Silvio Monfardini, MD, Lodovico Balducci, MD, Janine Overcash, PhD, APRN-CNP, FAANP, FAAN, and Matti S. Aapro, MD
Tweet this quote
However, outcomes in people aged 60 and older were still dismal, with lower remission rates, higher risks of treatment-related mortality, and increased risks of recurrence after remission. These initial studies provided a number of important hints for geriatric oncology.14 They raised the question of whether aging was a poor prognostic factor because the disease of older individuals was refractory to treatment, or because increased age was associated with a reduced tolerance of a strenuous chemotherapy regimen. They also revealed that a number of age-related conditions, such as myelodysplasia, predisposed individuals to the development of AML. They stimulated the search for less aggressive treatments, such as low-dose cytarabine. But perhaps most important, these studies showed the discrepancy between chronologic age and physiologic age in terms of resilience. Although prognosis was poorer for individuals aged 60 and older, chronologic age was not a reliable parameter to predict individual outcomes.
Around the same time, new insights into the immunology of aging suggested that age was a predisposing factor for the development of multiple myeloma. In 1960, Waldenstrom et al described the association of monoclonal gammopathy of unknown significance (MGUS) and aging, and in 1978 Kyle et al recognized MGUS as a precursor of multiple myeloma.15,16
The discovery of curative treatment of large-cell lymphoma (then named diffuse histiocytic lymphoma) and the adoption of adjuvant chemotherapy for breast cancer also had a major influence on geriatric oncology.
In 1974, the combination of cyclophosphamide, hydroxydaunorubicin, oncovin, and prednisone (CHOP) induced a complete remission in 60% of the cases of large-cell lymphoma, and 40% of patients were long-term survivors. Results were inferior for individuals aged 65 and older, who had been treated with a 50% reduction in the initial doses of cyclophosphamide and doxorubicin and gradual escalation of subsequent doses.17 A retrospective analysis of the data showed that older patients who had received the full dose of treatment had an outcome comparable to that of younger patients.
During the 1970s, two seminal studies of adjuvant chemotherapy for breast cancer were conducted. The Istituto Nazionale dei Tumori in Milan, Italy,18 conducted a randomized controlled trial of the combination of cyclophosphamide, methotrexate, fluorouracil (CMF) following a full resection of the breast cancer and axillary lymph nodes, whereas the National Surgical Adjuvant Breast Project compared single-agent melphalan with observation in women aged 70 and younger.19 Both studies showed that only premenopausal women benefited from adjuvant chemotherapy in terms of overall survival and disease-free survival. However, a retrospective review of the CMF data 20 years later showed that the benefits were extended to older women if they received at least 75% of the chemotherapy dose intensity.
Another important observation of those years was the report that cytotoxic chemotherapy may be a carcinogen itself.20 Eventually, it would be recognized that older individuals are particularly susceptible to developing a second malignancy.21
The Past History: Early Progress in the Treatment of Older Adults With Cancer
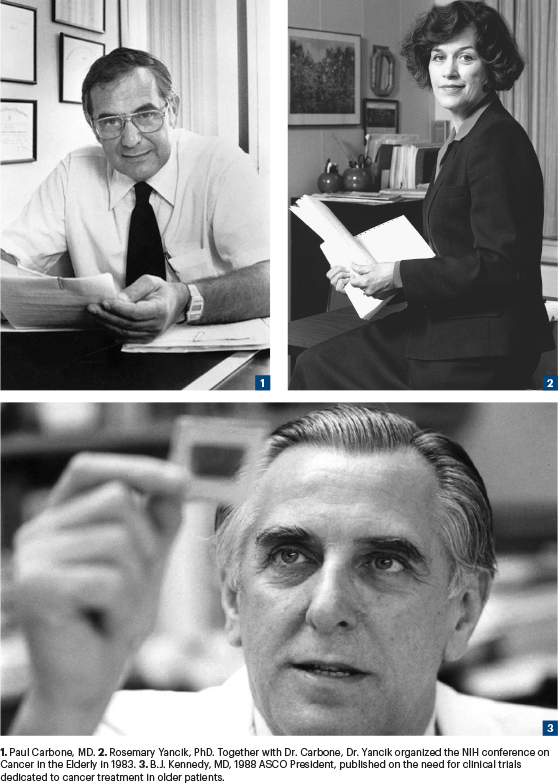
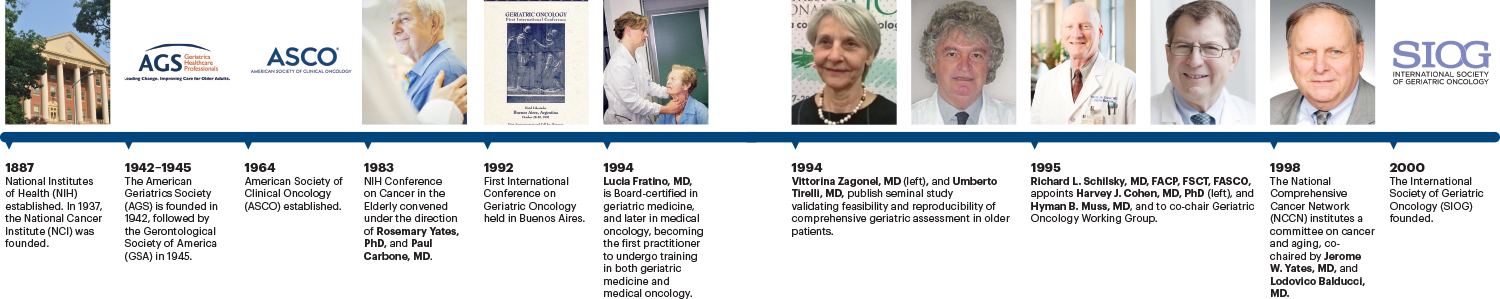
We begin the immediate past history of geriatric oncology with the conference on Cancer in the Elderly, organized in 1983 by Rosemary Yancik, PhD, and Paul Carbone, MD, at the National Institutes of Health (NIH),9 and end with the founding of the International Society of Geriatric Oncology (SIOG) in 2000. The conference on Cancer in the Elderly promoted worldwide interest in geriatric oncology, and the establishment of the SIOG provided a worldwide organization focused on the geriatric oncology movement. The NIH conference stressed the importance of a multidisciplinary approach to geriatric oncology. The SIOG embraced this multidisciplinary approach, and its members include geriatricians; medical, surgical, and radiation oncologists; nurses; and other health-care providers who are involved in the management of older adults with cancer.
In the 1980s, individuals older than age 65 in the United States accounted for 12% of the population and 50% of people diagnosed with cancer. Projections of cancer incidence then suggested that by 2030, 70% of all neoplasms would have occurred in the aged.22
The conclusions from the milestone Cancer in the Elderly conference were well summarized by Rao et al23 over 10 years ago. “This conference was attended by now-known pioneers in the field of geriatric oncology, who addressed a number of important issues, including existing discrepancies between physiologic and chronologic age; changes in age structure of the nation’s population and cancer control in the elderly; the role of cancer prevention and treatment in older adults; and approaches to increase the knowledge base in geriatric oncology by analyzing existing databases, conducting prospective clinical trials, initiating epidemiologic and longitudinal studies, evaluating the pharmacokinetics and chemosensitivity of drugs in older patients with cancer, evaluating and optimizing quality of life in older adults with cancer, and evaluating physician performance measures. The biology of aging and cancer was also discussed, and an increase in research using an interdisciplinary team approach was recommended”
Four outcomes were spawned from the conference over the next 2 decades (see timeline). Similar conclusions were drawn at the Joint NCI–European Organization for Research and Treatment of Cancer (EORTC) Consensus meeting on Neoplasia in the Elderly held in 1990. Since then, the United States and Europe have committed to integrating geriatric evaluation into oncology decision-making and treatment guidelines.
The Unwarranted Exclusion of Older Patients in Clinical Trials
Inspired by the dismal outcomes of AML in older patients, beginning in the 1980s, several studies addressed the issue of treatment toxicity and age. The results have been largely inconclusive. The report by Begg and Carbone deserves special mention.1
The authors examined the database from the Eastern Cooperative Oncology Group, including 19 trials of advanced cancer and 8 disease sites. Their conclusion was that individuals aged 70 and older were not at higher risk of treatment-related toxicity than younger patients, with the possible exception of neutropenia and thrombocytopenia. Of course, patients in these studies were highly selected in terms of functional status and comorbidity, and participants 80 years and older were scarce. Still, based on these data, it did not appear justified to reduce the dose intensity of chemotherapy in older patients or to exclude them from cancer clinical trials. Discrimination in clinical research based on chronologic age was unwarranted.
The same conclusions were reached by -Borkowski et al24 after reviewing a number of phase I trials conducted at the Johns Hopkins Oncology Center. According to the studies’ results, older adults should not be excluded from phase I trials on the basis of age alone, although only a small number of patients aged 75 years and older participated in these studies, with the oldest patient being 77. Bannon et al25 reported similar findings when reviewing patients aged 65 and older treated in phase II studies at the Illinois Cancer Center. Monfardini et al concurred with these results after reviewing the records of patients treated in phase II studies within the EORTC.26
For the first time, the authors of this report issued a word of caution: “Although age did not appear a justifiable exclusion criterion from clinical trials, this consideration pertained only to selected patients. It became imperative to assess physiologic age.” Other studies reported that older patients were at increased risk of treatment-related deaths,27 myelotoxicity, mucositis,28 cardiotoxicity,29 and peripheral and central neurotoxicity.30 In the meantime, investigators explored aging effects on pharmacokinetics26,27 and hemopoiesis,31 the most common target of chemotoxicity.
Assessing the Effects of Aging on Cancer and Its Treatment
Although early study findings produced divergent results, they allowed us to draw the following conclusions:
- Chronologic age (at least up to age 80) in and of itself was not an indicator of increased risk of chemotherapy-related -complications.
- Age was associated with pharmacologic changes that might have increased the risk of chemotherapy complications.
- The main challenge ahead for geriatric oncology was the determination of a patient’s resilience as it pertains to functional age.
The importance of considering functional age in the recruitment of patients into clinical trials was highlighted by the demonstration that older patients were underrepresented in cancer trials.1-4 As stated earlier, although individuals aged 65 and older accounted for 50% of patients with cancer, they accounted for only 20% of the clinical trial population, and the rate of participation in clinical trials decreased progressively with increasing age. Despite the mounting interest in geriatric oncology, the recruitment of older patients in cancer clinical trials remained low during the 1990s and early 2000s.3,4
These study results were consequential because they led to a number of strategies that improved the enrollment of older patients into clinical trials.32 Major steps of historical interest include the decision by Medicare to cover the cost of treatment in clinical trials33 and the changes in recruitment criteria, which became less stringent, allowing selection of patients with some degree of comorbidity and organ dysfunction to participate in clinical studies.34 Germane to the issues of prognosis and participation in clinical trials were questions related to the presentation of cancer in older adults, the pattern of care availability in the community, and the prevalence of comorbidity that might have increased the risk of mortality and impaired treatment tolerance in these older patients.
Old registry studies summarized by Goodwin and Samet35 showed that most cancers were diagnosed at a more advanced stage in older patients. There has been a lot of speculation concerning this finding, which is still an active area of research. It also became clear that older individuals were less likely to receive adequate treatment for their cancers. This was especially true for patients with locoregional and metastatic cancer,36,37 but even the risk of receiving inadequate treatment of localized disease increased with age and was as high as 52% in women aged 85 and older with stage II breast cancer.38
“Although age did not appear a justifiable exclusion criterion from clinical trials, the consideration pertained only to selected patients. It became imperative to assess physiologic age.”— Silvio Monfardini, MD, Lodovico Balducci, MD, Janine Overcash, PhD, APRN-CNP, FAANP, FAAN, and Matti S. Aapro, MD
Tweet this quote
The studies of comorbidity as a competitive cause of death flourished in the 1990s, the result of the ability to match information in the Surveillance, Epidemiology, and End Results (SEER) databases with the information in Medicare databases, which allowed investigators to identify the number and type of concomitant conditions in Medicare beneficiaries.39,40 Comorbidity might have provided an important competitive cause of death in patients with early stages of cancer, whereas comorbidity was less relevant to mortality in patients with advanced cancer.
This conclusion varied with the nature and seriousness of the comorbidity and the type of cancer. For example, certain concomitant conditions represented a relevant cause of mortality in patients with metastatic cancers that were associated with years of survival, including hormone-sensitive breast and prostate cancers. Also, this view of comorbidity needs to be revisited due to modern forms of antineoplastic treatment, which may now prolong the survival of patients with metastatic cancer for years compared with a few months. The studies of comorbidity in cancer of the head and neck by Piccirillo et al deserve a special mention here, because he included comorbidity as a prognostic and predictive factor in the staging of cancer of the upper airways in his studies.41
Still to be resolved is the issue of which comorbidity scale to use when calculating an individual patient’s comorbidities for clinical prognosis42: the Charlson Comorbidity Index, which assigns a weight to each comorbid condition based on the relative risk, or the Cumulative Illness Rating Scale–Geriatric (CIRS-G), which measures morbidity burden in the elderly. Ideally, in prospective studies, a scale such as CIRS-G, which takes into consideration the severity of chronic diseases, should be adopted.
Reducing the Risk of Treatment-Related Toxicities
A number of phase II trials were conducted to investigate reducing the risk of chemotherapy-related toxicity and mortality in older patients diagnosed with large-cell lymphoma. Three basic approaches were followed:
1. The elimination of anthracyclines from the treatment regimen pivoted by Tirelli43 in 1984, who used teniposide in lieu of doxorubicin.
2. The substitution of an anthracycline with -mitoxantrone.44-46
3. The use of lower doses of cytotoxic drugs in weekly treatment regimens.47,48
All of these approaches reported promising results validated by a retrospective study of 137 patients aged 70 and older treated at over a dozen EORTC institutions. The study suggested that patients treated with less toxic regimens had comparable outcomes to those treated with standard CHOP, with a reduced risk of complications.49
Eventually three randomized controlled studies showed that the use of standard CHOP in older individuals was superior to three non–doxorubicin-containing regimens.50-52 The results from the studies of large-cell lymphoma in older patients taught us three lessons of consequence in geriatric oncology:
1. Large randomized controlled studies were feasible in individuals aged 70 and older.
2. Less toxic forms of chemotherapy were available to older patients who could not tolerate standard treatments.
3. An assessment of functional age was necessary to determine the best candidates for aggressive treatment.
We would also add the results from a study by Zinzani et al,44 which demonstrated the amelioration of neutropenia and neutropenic infections with filgrastim in patients aged 70 and older.
Development of Randomized Clinical Studies in the Elderly
Results from studies showed that the prognosis of AML worsened after age 60. At the beginning of the 1980s, researchers tried to address the question of whether older individuals were able to tolerate aggressive induction regimens with cytarabine and an anthracycline. Several phase II studies tried to establish the benefit of less aggressive treatments in these patients, including attenuated doses of standard chemotherapy,53 low-dose cytarabine,54 or combination non-cytarabine and non-anthracycline chemotherapy.55 Randomized controlled studies were conducted in patients aged 60 and older to compare the benefit of aggressive vs dose-reduced induction therapy,56 the value of consolidation and maintenance treatments,57 and the benefit of post-remission induction hematopoietic growth factors.58,59

Today, these studies provide mainly historical interest since they confirm the feasibility of randomized controlled trials of AML in this age population and the potential benefits of some aggressive treatments in some older patients. As was the case with lymphoma, an assessment of functional age was wanted.
Perhaps the first prospective randomized study of cytotoxic chemotherapy in older patients with solid tumors was conducted by the Elderly Lung Cancer Vinorelbine Italian Study Group.60 The investigators randomized patients aged 70 and older with metastatic non–small cell lung cancer and an Eastern Cooperative Oncology Group (ECOG) performance status of up to 2 to receive either vinorelbine or best supportive care. The results demonstrated that chemotherapy was associated with better symptom control, survival, and quality of life. This study, led by Cesare Gridelli, MD, and supported by Dr. Monfardini, led the way for randomized controlled studies in the treatment of solid tumors in older patients.
Two prospective studies in the late 1990s represent a milestone toward the functional assessment of older patients in cancer clinical trials. In 1996, -Monfardini61 et al validated a multidimensional assessment in individuals aged 70 and older. And, in 1998, Extermann et al62 reviewed the 5-year results of the Senior Adult Oncology -Program at the Moffitt Cancer Center, in which patients aged 65 and older routinely underwent a comprehensive geriatric assessment. The study authors demonstrated that comorbidity and disability were independent variables compared with the classical Zubrod Scale performance status and might have had an independent value on predicting treatment tolerance and survival. These studies showed, respectively, that a comprehensive geriatric assessment was feasible and necessary for older patients with cancer, and they initiated some of the most consequential clinical investigations in geriatric oncology.
The 1990s: Establishing Research Priorities in Geriatric Oncology
Probably the first concerted effort to study geriatric oncology was the U.S. Department of Veterans Affairs Geriatric Research Education and Clinical Center (GRECC) in Little Rock, Arkansas. The activities at GRECC included the publication of a seminal article in the Annals of Internal Medicine,63 which provided a blueprint for research in the field of gerontology oncology and recommended the cooperation of different disciplines, and the attempt to establish a committee on cancer and age within the South West Oncology Group. As a result of those efforts, today, all major cooperative groups have a committee on aging.
Other notable efforts include the following:
1991—The establishment of a special interest group on aging and cancer within the American Geriatric Society, instituted by Dr. Balducci. The goal of this group then and now is to develop interest in oncology problems in the geriatric patient population.
1992—The EORTC Neoplasia in the Elderly Study Group was launched in Brussels, with Dr. Monfardini as Chairman. The main goal of this committee was to facilitate the enrollment of older patients into clinical trials. That same year, the first subcommittee on aging was installed within ECOG, co-chaired by William B. Ershler, MD, and Dr. Balducci.
1993—The National Cancer Institute in Aviano, Italy, hired a geriatrician to provide a comprehensive geriatric assessment of older patients.
1994—Lucia Fratino, MD, became board certified in geriatric medicine, and in 2000, she became board certified in medical oncology at the Medical School of Padua University, Italy. She is the first practitioner to undergo training in both geriatric medicine and medical oncology.
1994—Lodovico Balducci, MD, launched the first geriatric oncology program at Moffitt Cancer Center in Tampa, Florida.
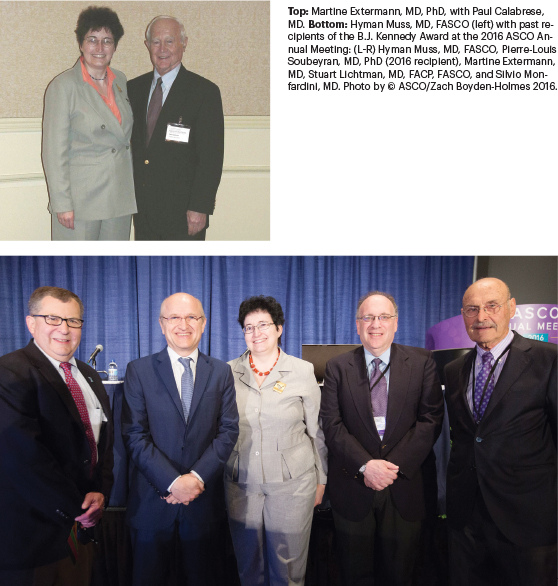
1995—Martine Extermann, MD, PhD, became a member of the Senior Adult Oncology Program at Moffitt Cancer Center and is now its program leader. She has published research showing the need to assess disability and comorbidity in addition to performance status in older patients with cancer.62
1995—Harvey J. Cohen, MD, PhD, now Director of the Center for the Study of Aging and Human Development and Walter Kempner Professor of Medicine at Duke University Medical Center, proposed the concept of a geriatric oncology working group to then Chair of the Cancer Acute Leukemia Group B (CALGB), Richard L. Schilsky, MD, FACP, FSCT, -FASCO, now Chief Medical Officer and Executive Vice President of ASCO, to focus attention and research on elderly patients with cancer.
1985—Dr. Schilsky appointed Dr. Cohen and Hyman B. Muss, MD, FASCO, now Mary Jones Distinguished Professor of Geriatric Oncology and Director of the Geriatric Oncology Program at the UNC Lineberger Comprehensive Cancer Center, to co-chair this new working group. Other members included researcher Alice B. Kornblith, PhD; Stuart M. Lichtman, MD, FACP, FASCO, medical oncologist at Memorial Sloan Kettering Cancer Center; Merrill J. Egorin, MD, now deceased; M. Margaret Kemeny, MD, FACS, Director of the Queens Cancer Center; MD; and Richard M. Stone, MD, Clinical Director of the Adult Leukemia Program at Dana-Farber Cancer Institute.
1995—The first study produced by the CALGB working group demonstrated that women aged 65 and older diagnosed with cancer were as willing as younger women to participate in clinical trials, but that investigators were less likely to offer trials to older women.64
1997—Jean-Pierre Droz, MD, organized a group of geriatric oncology consultations at the Centre Leon Berard in Lyon, France. The important work of this group in the development of the field of geriatric oncology includes the establishment of geriatric oncology in France and the promotion of the field worldwide. The group’s achievements were recently chronicled in the Journal of Geriatric Oncology.65
The History of Geriatric Oncology Publications and Conferences
1990—A group of seven medical oncologists from Guy’s Hospital in London, published “Cancer in the Elderly: Why So Badly Treated?” in The Lancet.70 The article detailed the enormity of the problem and inspired many young investigators and clinicians to join the field of geriatric oncology.
1990—A joint meeting by the National Cancer Institute and EORTC is held on neoplasia in the elderly in San Servolo Island, Venice.
1991—Former President of ASCO (1988) Byrl James “B.J.” Kennedy, MD, published an article in the -Journal of Clinical Oncology on the need for clinical trials dedicated to the investigation of cancer treatment in older patients and demonstrated the value of weekly modification of CHOP in the management of patients with lymphoma.71 In 1988, during his Presidential address, which he dedicated to cancer and aging, Dr. Kennedy emphasized the importance of focusing attention on the study of geriatric oncology.
1992–2000—Three textbooks on geriatric oncology are published, which organized the field and highlighted major research concerns, and help determine physiologic age as the most urgent key to defining the practice of geriatric oncology. The first one is Geriatric Oncology, edited by Lodovico Balducci, Gary G. Lyman, and William B. Ershler and published by Lippincott in 1992. The second isCancer in the Elderly: Treatment and Research, edited by Ian Fentiman and Silvio Monfardini and published by Oxford University Press in 1994.66 The third oneis Comprehensive Geriatric Oncology by Lodovico Balducci, William B. Ershler, and Gary H. Lyman, by Hardwood Press in 1997, and provides an extensive review of the effects of aging on the tolerance of cancer prevention, treatment, and the influence of age on treatment choice.
1997—Comprehensive Geriatric Oncology by Lodovico Balducci, MD, William B. Ershler MD, and Gary H. Lyman, MD, (Hardwood Press) is published and provides an extensive review of the effects of aging on the tolerance of cancer prevention, treatment, and the influence of age on treatment choice.
1997—In the 1990s, the Harford Foundation launched a series of seminars on geriatric education. Among the most successful of these conferences was one on geriatric oncology held in Puerto Rico in 1997 and awarded fellowships to seven major cancer centers in the United States.
1998—The National Comprehensive Cancer
Network institutes a committee on cancer and aging, co-chaired by Jerome W. Yates, MD, now Clinical Professor Emeritus at the State University of New York and Roswell Park Cancer Center, and Lodovico Balducci, MD, and issues the first guidelines on the management of cancer in older patients.67,68
Watch for Part 2 of the History of Geriatric Oncology in an upcoming issue of The ASCO Post.
Disclosure: The authors reported no conflicts of interest.
Dr. Monfardini is Director of the Geriatric Oncology Program at Instituto Palazzolo, Fondazione Don Gnocchi, in Milan, Italy. Dr. Balducci is Professor of Oncology and Medicine at the University of South Florida College of Medicine and Chief of the Division of Geriatric Oncology, Senior Adult Oncology Program at H. Lee Moffitt Cancer Center & Research Institute. Dr. Overcash is Professor of Clinical Nursing and Co-Director of the Academy for Teaching Innovation, Excellence and Scholarship. Dr. Aapro is Member of the Board, Genolier Cancer Center in Genolier, Switzerland, and of the International Society of Geriatric Oncology (SIOG) until September 2020.
References
1. White MC, Holman DM, Goodman RA, et al: Cancer risk among older adults: Time for cancer prevention to go silver.The Gerontologist 59(suppl 1):S10S6, 2019.
2. Begg CB, Carbone PP: Clinical trials and drug toxicity in the elderly. The experience of the Eastern Cooperative Oncology Group. Cancer 52:1986-1992, 1983.
3. Cohen HJ, Barolucci A: Age and the treatment of multiple myeloma. Southeastern Cancer Study Group experience. Am J Med 79:316-324, 1985.
4. Hutchins LF, Unger JM, Crowley JJ: Underrepresentation of patients 65 years of age or older in cancer-treatment trials. N Engl J Med 341:2061-2067, 1999.
5. Lewis JH, Kilgore ML, Goldman DP, et al: Participation of patients 65 years of age or older in cancer clinical trials. J Clin Oncol 21:1383-1389, 2003.
6. Talarico L, Chen Z, Pazdur R: Enrollment of elderly patients in clinical trials for cancer drug registration: A 7-year experience by the US Food and Drug Administration. J Clin Oncol 22:4626-4631, 2004.
7. Crimmins EM: Lifespan and healthspan: Past, present, and promise. Geronotologist 55:901-911, 2015.
8. Arai H, Ouchi Y, Yokode M, et al: Toward the realization of a better aged society: Messages from gerontology and geriatrics. Geriatr Gerontol Int 12:16-22, 2012.
9. Yancik R, Ries LA: Cancer in the older person. An international issue in an aging world. Semin Oncol 31:128-136, 2004.
10. Yancik R, Carbone PP: Perspectives on Prevention and Treatment of Cancer in the Elderly. New York, Raven Press, 1983.
10A. Perlia CT, Taylor SG: Hormonal treatment of breast cancer. Med Clin North Am 47:159-167, 1963.
11. Freireich EJ: Management of acute leukemia. Can Med Assoc J 96:1605-1610, 1967.
12. Ellison RR, Carey RW, Holland JF: Continuous infusion of arabynosil cytosine in patients with neoplastic diseases. Clin Pharmacol Ther 8:800-809, 1967.
13. Freireich EJ, Bodey GP, Harris GA, et al: Therapy of acute granulocytic leukemia. Cancer Res 27, 2573-2577, 1967.
14. Ballester OF, Balducci L, Saba HI: Acute myelogenous leukemia in older persons, in Balducci L, Lyman GH, ErshlerWB (eds): Geriatric Oncology, pp 223-231. Philadelphia, Lippincott, 1992.
15. Waldenström J: Studies on conditions associated with disturbed gamma globulin formation (gammopathies). Harvey Lect 56:211–231, 1960-1961.
16. Kyle RA: Monoclonal gammopathy of undetermined significance. Natural history in 241 cases. Am J Med 64:814–826, 1978.
17. Dixon DO, Neilan B, Jones SE, et al: Effect of age on therapeutic outcome in advanced diffuse histiocytic lymphoma. J Clin Oncol 4: 295-305, 1986.
18. Bonadonna G, Valagussa P, Moliterni A, et al: Adjuvant cyclophosphamide, methotrexate, and fluorouracil in node-positive breast cancer. N Engl J Med 332:901-906, 1995.
19. Fisher B; Carbone P; Economou SG, et al: 1-Phenylalanine mustard (L-PAM) in the management of primary breast cancer. A report of early findings. N Engl J Med 292:117-122, 1975.
20. Bonadonna G, DeLena M, Banfi A, et al: Secondary neoplasms inmalignant lymphoma after intensive chemotherapy. N Engl J Med 288:1242-1243, 1973.
21. Chaplain G, Milan C, Sgro C, et al: Increased risk of acute leukemia after adjuvant chemotherapy for breast cancer: A population-based study. J Clin Oncol 18: 2836-2842, 2000.
22. Yancik R, Ries LA: Cancer in older persons: Magnitude of the problem—How do we apply what we know? Cancer 74:1995-2003, 1994.
23. Rao VS, Garimella V, Hwang M, et al: Management of early breast cancer in the elderly. Int J Cancer 120:1155-1160, 2007.
24. Borkowski JM, Duerr M, Donehower RC, et al: Relation between age and clearance rate of nine investigational anticancer drugs from phase I pharmacokinetic data. Cancer Chemother Pharmacol 33:493-496, 1994.
25. Giovanazzi-Bannon S, Rademaker A, Lai G, et al: Treatment tolerance of elderly cancer patients entered onto phase II clinical trials: An Illinois Cancer Center study. J Clin Oncol11:2447-2452, 1994.
26. Monfardini S, Sorio R, Boes GH, et al: Entry and evaluation of elderly patients in European Organization for Research and Treatment of Cancer (EORTC) new-drug-development studies. Cancer 76:333-338, 1995.
27. Armitage JO, Potter JF: Aggressive chemotherapy for diffuse histiocytic lymphoma in the elderly: Increased complications with advancing age. J Am Geriatr Soc 32: 269-273, 1984.
28. Gelman RS, Taylor SG: Cyclophosphamide, methotrexate, and 5-fluorouracil chemotherapy in women more than 65 years old with advanced breast cancer. J Clin Oncol 2:1404-1413, 1984.
29. Robert J, Hoerni B: Age dependence of the early phase pharmacokinetic of doxorubicin. Cancer Res 43:4467-4469, 1983.
30. Robert J, Hoerni B: Age dependence of the early phase pharmacokinetic of doxorubicin. Cancer Res 43:4467-4469, 1983.
31. Hardy CL, Balducci L: Hemopoietic alterations of cancer. Am J Med Sci 290:196-205, 1985.
32. Singh H, Hurria A, Klepin HD: Progress Through Collaboration: An ASCO and U.S. Food and Drug Administration Workshop to Improve the Evidence Base for Treating Older Adults With Cancer. Am Soc Clin Oncol Educational Book 38:392- 399, 2018.
33. Unger JM, Coltman CA Jr, Crowley JJ: Impact of the year 2000 Medicare policy change on older patient enrollment to cancer clinical trials. J Clin Oncol 24:141-144, 2006.
34. Lichtman SM, Harvey RD, Damiette Smit MA; Modernizing Clinical Trial Eligibility Criteria: Recommendations of the American Society of Clinical Oncology-Friends of Cancer Research Organ Dysfunction, Prior or Concurrent Malignancy, and Comorbidities Working Group. J Clin Oncol 35:3753-3759, 2017.
35. Goodwin JS, Samet JM: Factors affecting the diagnosis and treatment of older cancer patients, in Balducci L, Lyman GH, Ershler WB (eds): Geriatric Oncology. Philadelphia, Lippincott, 1992.
36. Goodwin JS, Samet JM, Hunt WC: Determinants of survival in older cancer patients. J Natl Cancer Inst 88:1031-1038, 1996.
37. Newcomb PA, Carbone PP: Cancer treatment and age: Patient perspectives, J Natl Cancer Inst 85:1580-1584, 1993.
38. Goodwin JS, Samet JM: Care received by older women diagnosed with breast cancer. Cancer Control 4:313-319, 1994.
39. Yancik R, Ershler W, Satariano W, et al: Report of the national institute on aging task force on comorbidity. J Gerontol A Biol Sci Med Sci 62:275-280, 2007.
40. Satariano WA: Aging: Comorbidity and breast cancer survival: An epidemiologic view. Adv Exper Med Biol 330:1-11, 1993.
41. Piccirillo JF, Vlahiotis A, Barrett LB, et al: The changing prevalence of comorbidity across the age spectrum. Crit Rev Oncol Hematol 67:124-132, 2008.
42. Extermann M: Measurement and impact of comorbidity in older cancer patients. Crit Rev Oncol Hematol 35:181-200, 2000.
43. Tirelli U, Carbone A, Crivellari D, et al: A phase II trial of teniposide (VM 26) in advanced non-Hodgkin’s lymphoma, with emphasis on the treatment of elderly patients. Cancer 54:393-396, 1984.
44. Zinzani PL, Storti S, Zaccaria L, et al: Elderly aggressive-histology non-Hodgkin’s lymphoma. Blood 94:33-38, 1999.
45. Tirelli U, Zagonel V, Errante D, et al: A prospective study of a new combination chemotherapy regimen in patients older than 70 years with unfavorable non-Hodgkin’s lymphoma. J Clin Oncol 10:228-236, 1992.
46. Sonneveld P, Michiels JJ: Full dose chemotherapy in elderly patients with non-Hodgkin’s lymphoma. Br J Cancer 62:105-108, 1990.
47. O’Reilly SE, Connors JM, Howdle S, et al: In search of an optimal regimen for elderly patients with advanced-stage diffuse large-cell lymphoma. J Clin Oncol 11:2250-2257, 1993.
48. Martelli M, Guglielmi C, Coluzzi S, et al: P-VABEC: A prospective study of a new weekly chemotherapy regimen for elderly aggressive non-Hodgkin’s lymphoma. J Clin Oncol 11:2362-2369, 1993.
49. Tirelli U, Zagonel V, Serraino D, et al: Non-Hodgkin’s lymphomas in 137 patients aged 70 years or older. J Clin Oncol 6: 1708-1723, 1988.
50. Bastion Y, Blay JY, Divine M, et al: Elderly patients with aggressive non-Hodgkin’s lymphoma: Disease presentation, response to treatment, and survival. J Clin Oncol 15:2945-2953, 1997.
51. Tirelli U, Errante D, Van Glabbeke M, et al: CHOP is the standard regimen in patients 70 years of age [and older] with intermediate-grade and high-grade non-Hodgkin’s lymphoma. J Clin Oncol 16:27-34, 1998.
52. Sonneveld P, deRidder M, Van de Lelie H, et al : Comparison of doxorubicin and mitoxantrone in the treatment of elderly patients with advanced diffuse non-Hodgkin’s lymphoma using CHOP versus CNOP chemotherapy. J Clin Oncol 13:2530-2539, 1995.
53. Kahn SB, Begg CB, Mazza JJ, et al: Full dose versus attenuated dose daunorubicin, cytosine arabinoside, and 6-thioguanine in the treatment of acute nonlymphocytic leukemia in the elderly. J Clin Oncol 2:865-870, 1984.
54. Champlin RE, Gajewski TL,Golde DW: Treatment of acute myelogenous leukemia in the elderly. Sem Oncol 16:51-56, 1989.
55. Bow EJ, Sutherland JA, Kilpatrick MG, et al: Therapy of untreated acute myeloid leukemia in the elderly. J Clin Oncol 14:1345-1352, 1996.
56. Lowemberg B, Aittoun R, Kerkhof H, et al: On the value of intensive remission-induction chemotherapy in elderly patients of 65+ years with acute myeloid leukemia. J Clin Oncol 7:1268-1274, 1989.
57. Löwenberg B, Suciu S, Archimbaud E, et al: Mitoxantrone versus daunorubicin in induction-consolidation chemotherapy—the value of low-dose cytarabine for maintenance of remission, and an assessment of prognostic factors in acute myeloid leukemia in the elderly: Final report. J Clin Oncol 16:872-881
58. Löwenberg B, Suciu S, Archimbaud E,et al: Use of recombinant GM-CSF during and after remission induction chemotherapy in patients aged 61 years and older with acute myeloid leukemia. Blood 90:2952-2961, 1997.
59. Rowe JM, Andersen JW, Mazza JJ, et al; A randomized placebo-controlled phase III study of granulocyte-macrophage colony-stimulating factor in adult patients (> 55 to 70 years of age) with acute myelogenous leukemia. Blood 86:457-462, 1995.
60. Elderly Lung Cancer Vinorelbine Italian Study Group -(ELVIS): Effects of vinorelbine on quality of life and survival of elderly patients with advanced non-small-cell lung cancer. J Natl Cancer Inst 91:66-72, 1999.
61. Monfardini S, Ferrucci L, Fratino L, et al: Validation of a multidimensional evaluation scale for use in elderly cancer patients. Cancer 77:395-401, 1996.
62. Extermann M, Overcash J, Lyman GH, et al: Comorbidity and functional status are independent in older cancer patients. J Clin Oncol 16:1582-1587, 1998.
63. Lipschitz D, Goldstein S, Reis R, et al: Cancer in the elderly: Basic Sciences and Clinical Aspects. Ann Int Medicine 102:218-228, 1985.
64. Kemeny MM, Adak S, Gray B, et al: Combined-modality treatment for resectable metastatic colorectal carcinoma to the liver: Surgical resection of hepatic metastases in combination with continuous infusion of chemotherapy—An intergroup study. J Clin Oncol 15: 1499-1505, 2003.
65. Russo C, Terret C, Cropet C, et al: Geriatric assessment in oncology. Moving the concept forward. The 20-year experience at the centre Leon Berard Geriatric Oncology Program. J Geriatr Oncol 9:673-678, 2018.
66. Fentiman IS; Monfardini S: Cancer in the Elderly: Treatment and Research. New York, Oxford University Press, 1994.
67. Kennedy BJ: Needed: Clinical trials for older patients. J Clin Oncol 9:718-720, 1991.
68. Balducci L, Yates JW: General guidelines for the management of older patients with cancer. Oncology 14:221-227, 2000.

