In a randomized phase II trial (KEYNOTE-002) reported in The Lancet Oncology, Antoni Ribas, MD, of UCLA Jonsson Comprehensive Cancer Center, Los Angeles, and colleagues found that treatment with the anti–PD-1 (programmed cell death protein 1) antibody pembrolizumab (Keytruda) prolonged progression-free survival vs investigator-choice chemotherapy in patients with advanced melanoma progressing on ipilimumab (Yervoy) and, if BRAF V600-mutant positive, a BRAF or MEK inhibitor.1
Study Details
A total of 540 patients with progressive disease within 24 weeks after at least two ipilimumab doses and, if BRAF V600-mutant positive, previous treatment with a BRAF or MEK inhibitor or both took part in this open-label trial. They were randomized 1:1: between November 2012 and November 2013 to receive pembrolizumab 2 mg/kg (n = 180) or 10 mg/kg (n = 181) every 3 weeks or investigator-choice chemotherapy (n = 179, including 42 to paclitaxel plus carboplatin, 28 to paclitaxel, 13 to carboplatin, 45 to dacarbazine, and 43 to temozolomide).
Patients had to have resolution of all ipilimumab-related adverse events to grade 0 or 1 and prednisone ≤ 10 mg/d for at least 2 weeks. Randomization was stratified by Eastern Cooperative Oncology Group performance status, lactate dehydrogenase (LDH) concentration, and BRAF V600-mutation status. Patients were masked to the dose of pembrolizumab. The primary endpoint was progression-free survival in the intent-to-treat population.
Patients had a median age of 60 to 63 years, 96% to 99% were white, 58% to 64% were male, 54% to 55% had a performance status of 0, 76% to 78% had wild-type BRAF, 55% to 60% had normal LDH levels, 82% to 83% had stage M1c disease, 36% to 44% had two lines and 30% to 33% had at least three lines of prior therapy, 46% to 50% had received chemotherapy, and 24% to 26% had received a BRAF or MEK inhibitor.
Progression-Free Survival
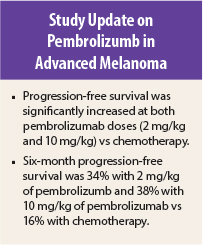
At the prespecified second interim analysis, at a median follow-up of 10 months, progression-free survival on independent central review was significantly prolonged in the pembrolizumab 2-mg/kg group (hazard ratio [HR] = 0.57, P < .0001) and in the pembrolizumab 10-mg/kg group (HR = 0.50, P < .0001) compared with the chemotherapy group. There was no significant difference for the 10-mg/kg dose vs the 2-mg/kg dose (HR = 0.91, 95% confidence interval [CI] = 0.71–1.16).
More than half of all patients had progressed by 12 weeks, the time of the first tumor assessment. Median progression-free survival was 2.9 months (95% CI = 2.8–3.8 months) and 2.9 months (95% CI = 2.8–4.7 months) in the pembrolizumab groups (2-mg/kg dose and 10-mg/kg dose, respectively) vs 2.7 months (95% CI = 2.5–2.8 months) in the chemotherapy group. Six-month progression-free survival was 34% (95% CI = 27%–41%) in the 2-mg/kg group and 38% (95% CI = 31%–45%) in the 10-mg/kg group vs 16% (95% CI = 10%–22%) in the chemotherapy group. In post hoc analysis, restricted mean progression-free survival was 5.8 and 6.5 vs 3.7 months, respectively.
The benefit of both pembrolizumab doses was observed in all prespecified subgroups, including BRAF and LDH status subgroups.
On independent central review, response was observed in 21% of patients in the pembrolizumab 2-mg/kg group and 25% of the 10-mg/kg group vs 4% of the chemotherapy group (P < .0001 for both comparisons). Overall survival analysis is awaited.
Adverse Events
The most common treatment-related grade 1 or 2 adverse events among pembrolizumab patients were fatigue (21% and 28% vs 32% of the chemotherapy group) and pruritus (21% and 23% vs 4% of the chemotherapy group); among patients receiving chemotherapy, nausea was the most common adverse event (30%, vs 4% and 8% in the pembrolizumab 2 mg/kg and 10 mg/kg groups).
Treatment-related grade 3 or 4 adverse events occurred in 11% of patients in the pembrolizumab 2-mg/kg group, 14% of the pembrolizumab 10-mg/kg group, and 26% of the chemotherapy group, with the most common in pembrolizumab patients being fatigue (1% and < 1% vs 5%) and the most common in the chemotherapy group being anemia (5%), fatigue (5%), neutropenia (4%), and leukopenia (4%). Treatment-related adverse events led to treatment interruption in 8%, 8%, and 18% of patients and treatment discontinuation in 3%, 7%, and 6%, respectively.
The investigators concluded: “These findings establish pembrolizumab as a new standard of care for the treatment of ipilimumab-refractory melanoma.” They noted that since available data do not indicate that one pembrolizumab dosing regimen is superior to another, the pembrolizumab dose of 2 mg/kg given every 3 weeks is recommended for further use. ■
Disclosure: The study was funded by Merck Sharp & Dohme. For full disclosures of the study authors, visit www.thelancet.com.
Reference
1. Ribas A, Puzanov I, Dummer R, et al: Pembrolizumab versus investigator-choice chemotherapy for ipilimumab-refractory melanoma (KEYNOTE-002): A randomised, controlled, phase 2 trial. Lancet Oncol. June 23, 2015 (early release online).