In the Clinic provides overviews of novel oncology agents, addressing indications, mechanisms, administration recommendations, safety profiles, and other essential information needed for the appropriate clinical use of these drugs.
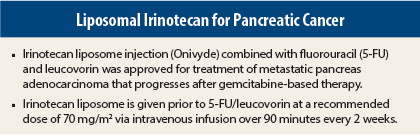
On October 22, 2015, irinotecan liposome injection (Onivyde) given in combination with fluorouracil (5-FU) and leucovorin was approved for treatment of metastatic pancreas adenocarcinoma progressing after gemcitabine-based therapy.1,2
Supporting Efficacy Data
Approval was based on the finding of improved overall survival in an open-label phase III trial where 417 patients were randomly assigned to receive irinotecan liposome at 70 mg/m2 with leucovorin at 400 mg/m2 and 5-FU at 2,400 mg/m2 over 46 hours every 2 weeks (n = 117), irinotecan liposome at 100 mg/m2 every 3 weeks (n = 147), or leucovorin at 200 mg/m2 and 5-FU at 2,000 mg/m2 over 24 hours weekly for 4 weeks followed by a 2-week rest (n = 134) until disease progression or unacceptable toxicity.2
Patients had to have serum bilirubin within the institutional normal range and albumin ≥ 3 g/dL. Patients homozygous for the UGT1A1*28 allele (which leads to accumulation of the active irinotecan metabolite) initiated treatment with irinotecan liposome at a reduced dose.
The trial was initiated as a two-arm study and subsequently amended to include the irinotecan liposome/5-FU/leucovorin arm. The efficacy comparisons between this arm and the 5-FU/leucovorin arm are limited to the 119 patients enrolled in the 5-FU/leucovorin arm after the amendment. For these two groups, patients had a median age of 63 years (range = 34–81 years; 41% ≥ 65 years); 58% were men, 63% were white, 30% were Asian, and 3% were black or African American. Karnofsky performance score was 90 to 100 in 53% of patients; 67% had liver metastasis and 31% lung metastasis; 13% had received gemcitabine only in the neoadjuvant/adjuvant setting; and 55% had received one prior line of therapy for metastatic disease, whereas 33% had at least two prior lines.
Median overall survival was 6.1 months in the irinotecan liposome plus 5-FU/leucovorin group vs 4.2 months in the 5-FU/leucovorin group (hazard ratio [HR] = 0.68, P = .014). Median progression-free survival was 3.1 vs 1.5 months (HR = 0.55, 95% confidence interval = 0.41–0.75). The objective response rate was 7.7% vs 0.8%. There was no improvement in overall survival for irinotecan liposome alone vs 5-FU/leucovorin (HR = 1.00, P = .97).
How It Works
Irinotecan liposome injection is a topoisomerase I inhibitor encapsulated in a lipid bilayer vesicle, or liposome. Topoisomerase I relieves torsional strain in DNA by inducing single-strand breaks. Irinotecan and its active metabolite (SN-38) bind reversibly to the topoisomerase I/DNA complex and prevent religation of the single-strand breaks, leading to exposure time-dependent double-strand DNA damage and cell death.
In mice with human tumor xenografts, irinotecan liposome given at irinotecan hydrochloride–equivalent doses fivefold lower than irinotecan hydrochloride achieved similar intratumoral exposure of SN-38.
How It Is Used
Irinotecan liposome is given prior to 5-FU/leucovorin at a recommended dose of 70 mg/m2 via intravenous infusion over 90 minutes every 2 weeks. The recommended starting dose in patients known to be homozygous for the UGT1A1*28 allele is 50 mg/m2, which can be increased to 70 mg/m2 as tolerated in subsequent cycles. There is no recommended dose for patients with serum bilirubin above the upper limit of normal. Patients should be premedicated with a corticosteroid and antiemetic 30 minutes before treatment.
Treatment should be withheld for diarrhea of grade ≥ 2. Intravenous or subcutaneous atropine at 0.25 to 1 mg should be given for early-onset diarrhea of any severity (unless clinically contraindicated) and loperamide for late-onset diarrhea of any severity.
Dose modifications for diarrhea and other grade 3 or 4 adverse events include withholding treatment until recovery to grade ≤ 1 and resumption at 50 mg/m2 (43 mg/m2 for patients with UGT1A1*28 allele receiving 50 mg/m2) for a first occurrence and 43 mg/m2 (35 mg/m2) for a second occurrence. Treatment should be discontinued for a third occurrence and for a first occurrence of interstitial lung disease or anaphylactic reaction.
Use of strong CYP3A4 inducers (eg, rifampin, phenytoin, carbamazepine, rifabutin, rifapentine, phenobarbital, St. John’s wort) should be avoided; non–enzyme-inducing therapies should be substituted at least 2 weeks prior to initiation of irinotecan liposome. Use of strong CYP3A4 inhibitors (eg, ketoconazole, clarithromycin, indinavir, itraconazole, lopinavir, nefazodone, nelfinavir, ritonavir, saquinavir, telaprevir, voriconazole) and strong UGT1A1 inhibitors (eg, ketoconazole, atazanavir, gemfibrozil, indinavir) should be avoided; strong CYP3A4 inhibitors should be stopped at least 1 week prior to starting therapy.
Safety Profile
Among the 117 patients in the irinotecan liposome plus 5-FU/leucovorin group and 134 in the 5-FU/leucovorin group, the most common adverse events of any grade were diarrhea (59%, including 30% with early and 43% with late diarrhea in the irinotecan liposome combination group, vs 26%, including 15% and 17% in the 5-FU/leucovorin group), fatigue/asthenia (56% vs 43%), vomiting (52% vs 26%), nausea (51% vs 34%), decreased appetite (44% vs 32%), stomatitis (32% vs 12%), and pyrexia (23% vs 11%); infection/infestation occurred in 38% vs 15%.
The most common grade 3 or 4 adverse events were fatigue/asthenia (21% with irinotecan liposome vs 10% without), diarrhea (13%, including early in 3% and late in 9%, vs 4%), vomiting (11% vs 3%), and nausea (8% vs 4%); grade 3 or 4 infection/infestation occurred in 17% vs 10%. The most common grade 3 or 4 laboratory abnormalities were lymphopenia (27% vs 17%) and neutropenia (20% vs 2%).
The most common serious adverse events in irinotecan liposome recipients (occuring in ≥ 2%) were diarrhea, vomiting, neutropenic fever or neutropenic sepsis, nausea, pyrexia, sepsis, dehydration, septic shock, pneumonia, acute renal failure, and thrombocytopenia. Adverse events led to irinotecan liposome dose reduction in 33% (most commonly due to neutropenia, diarrhea, nausea, and anemia), dose interruption or delay in 62% (most commonly due to neutropenia, diarrhea, fatigue, vomiting, and thrombocytopenia), and discontinuation in 11% of patients (most commonly due to diarrhea, vomiting, and sepsis).
Irinotecan liposome carries boxed warnings for severe neutropenia, including fatal neutropenic sepsis, and severe diarrhea. It should not be administered to patients with bowel obstruction.
Blood cell counts should be monitored during treatment. Irinotecan liposome also carries warnings/precautions for interstitial lung disease, including fatal cases, severe hypersensitivity reactions, and embryofetal toxicity. It is contraindicated in patients with severe hypersensitivity reaction to irinotecan liposome or irinotecan hydrochloride. Women should not breastfeed during irinotecan liposome treatment. ■
References
1. U.S. Food and Drug Administration: Irinotecan liposome injection. Available at www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm468728.htm. Accessed November 4, 2015.
2. Onivyde (irinotecan liposome injection) for IV use prescribing information, Merrimack Pharmaceuticals, Inc, October 2015. Available at www.accessdata.fda.gov/drugsatfda_docs/label/2015/207793lbl.pdf. Accessed November 4, 2015.