Prostate cancer has been slow to catch up with breast cancer in terms of using biomarkers, but a new study represents progress in this regard. A genomic classifier called Decipher® provides important information that can be used to make treatment decisions for men with prostate cancer and a rising prostate-specific antigen (PSA) after radical prostatectomy. The genomic classifier was able to distinguish between low-risk and high-risk men in this setting who received salvage radiation therapy (with or without hormonal therapy). Results were presented at the 2015 ASTRO Annual Meeting.1
“With current standard practice, many patients are both over- and undertreated. Our study shows that you can identify high-risk men based on a genomic classifier score who should get intensified therapy, while men identified as low-risk can safely defer further treatment,” said Robert Den, MD, of the Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia.
“Patients with a low genomic classifier score have an excellent prognosis with salvage radiotherapy and may avoid concurrent hormonal therapy. This group can safely delay salvage radiotherapy, whereas those with a high genomic classifier score are at significant risk of metastatic disease and may benefit from intensified systemic therapy. Integration of a genomic classifier into clinical practice can impact on decision-making for these men in the postprostatectomy setting,” Dr. Den said.
Genomic Platforms
Three RNA-based genomic platforms are currently commercially available for use in patients with prostate cancer. Genomic Prostate Score (GPS) is used prior to treatment, whereas Decipher is performed after surgical resection. The third test, Prolaris, can be used before or after surgery.
The Decipher test, which analyzes a small tissue sample obtained during prostatectomy, has been approved by Medicare for reimbursement. Dr. Den said he uses it routinely in his clinical practice and that it is being adopted across the country.
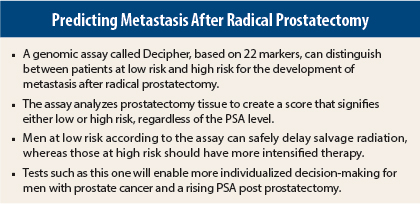
In an interview with The ASCO Post, Dr. Den explained that the Decipher platform uses a chip with 1.4 million markers containing coding and noncoding genes. The genomic classifier score is derived based on 22 markers that are involved in different parts of the metastatic pathway; Prolaris and GPS use a polymerase chain reaction approach looking at amplification of 31 and 12 genes, respectively.
“We have shown that there is predictive value in the set of 22 classifier genes. However, the Decipher platform also provides a view of the genome beyond the classifier genes, that may help inform future studies,” he noted.
Study Details
The retrospective study included 170 men treated with salvage radiation therapy at three different institutions: Thomas Jefferson, Duke University, and the Mayo Clinic. This was a multi-institutional and multiethnic cohort.
The median age of study patients was 61 years (range, 39–75 years). About 42% were Gleason 7 (3+4) and 24.7% were Gleason 7 (4+3). More than 30% of men were African American, who typically are not well represented in clinical trials. About 20% were on concurrent hormone therapy as part of their salvage treatment. Eighty percent had clear surgical margins following prostatectomy.
Salvage radiotherapy was defined as radiotherapy given if the PSA level was > 0.2 ng/mL or after salvage androgen-deprivation therapy. Early salvage radiation therapy was defined as given when the PSA level was 0.2–1 ng/mL, and late salvage radiation therapy was defined as given when the PSA level was >1 ng/mL.
The primary endpoint was the development of regional or distant metastasis, as documented on CT and/or bone scan. Biochemical failure was not used as a surrogate marker for metastatic disease.
Dr. Den and colleagues compared the genomic classifier with two different nomograms based on clinicopathologic features (Briganti and CAPRA-S); they found that Decipher was the most significant prognostic factor for the development of clinical metastases.
Risk Classification
Regardless of the PSA level, the study showed that in patients classified as low-risk by the genomic classifier score, there was no difference in the cumulative incidence of metastasis whether or not they had salvage radiation; in these patients, the rate of metastasis at 10 years was < 10%. In contrast, high-risk men who received early salvage radiation had a 15% cumulative incidence of metastasis at 10 years, whereas those treated with late salvage therapy had a 33% cumulative incidence of metastasis at this time point.
The study was not without limitations. It was a retrospective analysis and did not allow for analysis of cancer-specific mortality.
‘The Wave of the Future’
ASTRO Incoming President David Beyer, MD, of the Cancer Centers of Northern Arizona in Sedona, hailed these results as “the wave of the future.”
He continued: “This is an important study. I don’t know which of the genomic tests will turn out to be best, but in any event, we will be using tests like this to determine who needs intensified treatment and who doesn’t. The standard of care will be some type of test that will allow us to personalize management of prostate cancer.” ■
Disclosure: Dr. Den received an unrestricted grant from GenomeDx, the supporter of this study. Dr. Beyer reported no potential conflicts of interest.
Reference
1. Den RB, Choeurng V, Howard L, et al: Validation of a genomic classifier for prediction of metastasis following postoperative salvage radiation therapy. 2015 ASTRO Annual Meeting. Abstract 306. Presented October 21, 2015.