The use of hypofractionated intensity-modulated radiotherapy (IMRT) appears to be a reasonable option for men with intermediate- to high-risk prostate cancer,1 reported Alan Pollack, MD, Chairman of Radiation Oncology at the University of Miami Miller School of Medicine in Miami and lead investigator of the long-term Fox Chase trial. Five years after treatment, the shorter course of radiation treatment delivered via hypofractionated IMRT (in 2.5 weeks less time) was equally as effective as conventional IMRT in reducing biochemical failure in intermediate- to high-risk patients with prostate cancer.
 “We are still learning how best to apply hypofractionation, and the results in this trial show that the technique is very effective,” stated Dr. Pollack at the 53rd Annual Meeting of the American Society for Radiation Oncology (ASTRO) Plenary Session.
“We are still learning how best to apply hypofractionation, and the results in this trial show that the technique is very effective,” stated Dr. Pollack at the 53rd Annual Meeting of the American Society for Radiation Oncology (ASTRO) Plenary Session.
Between 2002 and 2006, a total of 307 patients took part in the study, with approximately half receiving conventional IMRT (76 Gy in 2.0 Gy fractions) and half receiving hypofractionated IMRT (70.2 Gy in 2.7 fractions). The high-risk patients also received hormone therapy for 2 years. Recurrences were determined by monitoring prostate-specific antigen levels. At 5 years after treatment, there was no significant difference in the rate of biochemical failure in the conventional and hypofractionated IMRT arms (about 22% each). Rates for locoregional failure/distant metastasis were 1.0% and 1.3%, respectively, for the conventional and hypofractionated IMRT arms at 5 years.
Genitourinary Toxicity
The rates of side effects were relatively low for both treatment methods, according to Dr. Pollack. There were identical long-term rates of bowel/rectal reactions and the frequency of unsatisfactory erections. Although the number of grade 2+ rectal reactions was “quite low,” there was a significant increase in the number of grade 2+ genitourinary reactions among those who received hypofractionation.
At 5 years, 8.3% of patients treated with conventional IMRT experienced late grade 2+ genitourinary reactions, compared with 18.3% of patients treated with hypofractionated IMRT. There also was significantly higher bladder control in the conventionally fractionated arm than patients receiving hypofractionated therapy.
“Late urinary symptoms were higher with hypofractionation but were low overall,” declared Dr. Pollack, “particularly when the incidence of persistent urinary symptoms (< 10% at 5 years) was analyzed.”
AUA Score
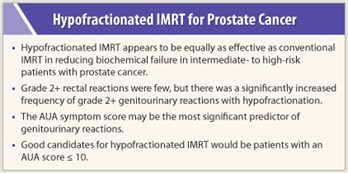 In addition, the role of the American Urological Association (AUA) symptom score was briefly explored. The median AUA score of study participants was 5. “We found the AUA symptom score to be the most significant predictor of genitourinary reactions, especially with > 10 being highly predictive of grade 2+ urinary side effects,” revealed Dr. Pollack. With the AUA pretreatment score being a strong determiner of outcome after fractionation, good candidates for hypofractionaed IMRT would have an AUA score ≤ 10.
In addition, the role of the American Urological Association (AUA) symptom score was briefly explored. The median AUA score of study participants was 5. “We found the AUA symptom score to be the most significant predictor of genitourinary reactions, especially with > 10 being highly predictive of grade 2+ urinary side effects,” revealed Dr. Pollack. With the AUA pretreatment score being a strong determiner of outcome after fractionation, good candidates for hypofractionaed IMRT would have an AUA score ≤ 10.
The study investigators believe that their findings justify the rationale for phase III trials of hypofractionated IMRT in this population with prostate cancer. Similar regimens are being tested in clinical trials, including the Cleveland Clinic study, and the results are eagerly awaited.
“Although [hypofractionated IMRT] is not yet adopted broadly because of the need for long-term follow-up, hypofractionation is rapidly gaining momentum for many types of cancer,” concluded Dr. Pollack. “The results presented here bring us much closer to effectively treating prostate cancer in a shorter period of time, with acceptable side effects.” ■
Disclosure: Dr. Pollack reported no potential conflicts of interest.
SIDEBAR: Expert Point of View: Hypofractionated Radiotherapy Effectively Controls High-risk Prostate Cancer
Reference
1. Pollack A, Walker G, Buyyounouski M, et al. Five year results of a randomized external beam radiotherapy hypofractionation trial for prostate cancer. 53rd ASTRO Annual Meeting. Abstract 1. Presented October 3, 2011.

 The take-home message of the study findings from the Fox Chase trial reported at the 53rd ASTRO Annual Meeting plenary session supports the use of hypofractionated intensity-modulated radiotherapy as a more convenient and cost-effective alternative than conventional IMRT, according to formal...
The take-home message of the study findings from the Fox Chase trial reported at the 53rd ASTRO Annual Meeting plenary session supports the use of hypofractionated intensity-modulated radiotherapy as a more convenient and cost-effective alternative than conventional IMRT, according to formal...