A new resource-stratified ASCO guideline update provides new evidence-based recommendations for the secondary prevention of cervical cancer in various resource settings.1 In the updated guideline, the screening recommendations cover basic, limited, enhanced, and maximal resource settings.
Since ASCO published the first resource-stratified cervical cancer screening guidelines in 2016, there have been several improvements in techniques and strategies for cervical cancer screening globally, explained Surendra S. Shastri, MBBS, MD, DPh, DHA, of The University of Texas MD Anderson Cancer Center and guideline Expert Panel Co-Chair.
Dr. Shastri explained that availability and access are the most important contributors to global disparities in cervical cancer control. “Until less than a decade ago, cytology was the only cervical cancer screening tool known,” he added. “Cytology requires highly trained personnel, including cytotechnologists and cytopathologists, and well-equipped laboratories, which were not available in resource-poor settings.”
Dr. Shastri added that new techniques like human papillomavirus [HPV] testing and visual inspection with acetic acid do not require multiple resources “and are equal or better with reference to sensitivity and specificity as compared to cytology.” He noted that these new screening tests “are now making cervical cancer screening available even in the lowest-resource settings.”
Jose Jeronimo, MD, of the National Cancer Institute and guideline Expert Panel Co-Chair, stated that given the rapid evolution of technology in cervical cancer prevention, there has been a significant need to update the 2016 ASCO guidelines. “In the 2016 guidelines, the evidence was just coming [out] for these new technologies,” he said. “The guidance for areas where most cervical cancer cases happen—the areas with very low resources—the recommendations for those areas are really very important to be updated and to accommodate these new technologies.”
According to Dr. Jeronimo, cervical cancer is “basically a marker of social disparity,” adding that many women who die of cervical cancer live in areas with considerably limited resources, limited access to health care, and limited access to screening for cancer. “And that’s the goal, trying to update to provide more state-of-the-art options for the different settings,” he said.
Updated Recommendations
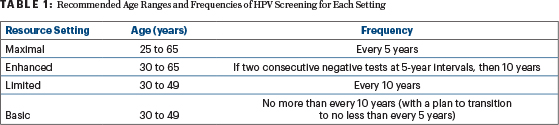
The primary recommendation made in the guideline states that either self- or clinician-collected HPV DNA testing should be used in all resource settings (Table 1). “HPV testing has the potential to become the primary screening test in all resource settings, reducing the frequency of screening, as well as the number of times one has to screen in their lifetime,” Dr. Shastri said.
Dr. Jeronimo stated that HPV testing has become more affordable in many places, making it a preferable strategy for a variety of resource settings. “There are new HPV technologies being implemented and are hopefully going to be cheaper in the future and more affordable for areas with limited resources,” he said.
Dr. Jeronimo added that findings from this type of testing may also mean less frequent testing is needed, which can be ideal in resource-constrained settings. “If a woman is negative for the virus, we know she will be very well protected for the next 10 years at least,” he explained, “which means we don’t need to screen those women who test negative that frequently.”
The updated guideline also discusses HPV self-collection, where the test kit is mailed to the homes of eligible individuals who collect their own samples and send them to the laboratory. Dr. Shastri stated this represents a “new and user-friendly innovation that has the potential to make cervical cancer screening available and accessible to most women globally, even in the poorest-resource settings.”
In addition, the guideline added that visual inspection with acetic acid can be employed in basic resource settings but encourages transitioning to population-based screening with HPV testing “at the earliest opportunity.”
Additional Updates and Future Considerations
The guideline panel made other updated recommendations for special populations, including the following:
- Women who are postpartum: Primary screening should be offered 6 weeks postpartum in basic settings and 6 months in other settings.
- Women who have received a total hysterectomy for benign causes with no history of cervical dysplasia or HPV: Screening may be discontinued.
- Women who have received a subtotal hysterectomy (with an intact cervix): Routine screening should continue.
Also, the guideline recommends that women who are positive for HIV or those who are immunosuppressed for other reasons should undergo screening with HPV testing as soon as diagnosed. The guideline recommends screening in this special population “twice as many times in a lifetime as the general population.”
Dr. Jeronimo noted there is still not a sufficient amount of data regarding screening women who are HIV-positive, adding that additional research is needed to better inform screening strategies in this special population. “One of the challenges [with screening] women who are HIV-positive [is that] they have some level of immunosuppression, [so] the infection with HPV is much more common,” he explained. “The kind of research to have a much better strategy for women who are HIV-positive is something that is lacking still in all the guidance I know, and something we are going to need to update in the future.”
In addition, Dr. Jeronimo commented that more people are being vaccinated against HPV than in previous years. “And because more women are already vaccinated, we don’t know how the screening is going to be in those vaccinated populations,” he said. “Maybe it’s going to be less frequent or maybe even once or twice in the lifetime, so that’s also something we need to look at in the future.”
REFERENCE
1. Shastri SS, Temin S, Almonte M, et al: Secondary prevention of cervical cancer: ASCO resource-stratified guideline update. J Clin Oncol. September 26, 2022 (early release online).
Originally published in ASCO Daily News. © American Society of Clinical Oncology. ASCO Daily News, September 28, 2022. All rights reserved.

