In patients with early resectable triple-negative breast cancer, not only did the addition of carboplatin to standard neoadjuvant chemotherapy improve pathologic complete response rates, it also improved 4-year event-free survival, regardless of BRCA status, according to the latest analysis of the phase III randomized BrighTNess trial.1

Sibylle Loibl, MD, PhD
“Overall, these findings support the inclusion of carboplatin into neoadjuvant chemotherapy for patients with stage II and III triple-negative breast cancer, regardless of germline BRCA status,” said Sibylle Loibl, MD, PhD, Chief Executive Officer and Chair of the German Breast Group. Presenting the new data at the European Society for Medical Oncology (ESMO) Congress 2021, she reported a 43% reduction in risk with the addition of carboplatin to paclitaxel (P = .02).
“Additionally, patients with pathologic complete responses had significantly better event-free survival, and this also was similar in patients with and without germline BRCA mutations,” Dr. Loibl noted.
BrighTNess also evaluated the benefit of adding veliparib, a poly (ADP-ribose) polymerase (PARP) inhibitor, to carboplatin, but this approach yielded no improvement in pathologic complete response rate, event-free survival, or overall survival, she said.
Study Details
The BrighTNess trial randomly assigned 634 patients with stage II or III operable triple-negative breast cancer to one of three arms: paclitaxel/carboplatin/veliparib (n = 316), paclitaxel/carboplatin (n = 160), or paclitaxel alone (n = 158). All treatments were followed by four cycles of doxorubicin and cyclophosphamide, with surgery performed 2 to 8 weeks after the last chemotherapy dose. The primary endpoint was pathologic complete response. Event-free survival, overall survival, and safety were secondary endpoints.
In the previously reported primary analysis, paclitaxel/carboplatin/veliparib was superior to paclitaxel alone but was not superior to paclitaxel/carboplatin (without veliparib).2 Because of the statistical design of the study, the subsequent secondary analyses are descriptive, with nominal P value, she said.
Carboplatin, with or without veliparib, significantly improved pathologic complete response compared with standard neoadjuvant chemotherapy alone: 53% and 58%, respectively, vs 31%. The finding of benefit with the addition of carboplatin to neoadjuvant therapy was supported by two other randomized trials: CALGB 40603/Alliance trial3 and GeparSixto,4,5 which also showed improvements in pathologic complete response rates with carboplatin. However, the impact of neoadjuvant carboplatin on long-term outcomes has remained unclear, she said.
“Here, we report long-term event-free survival, long-term overall survival, and the rate of second malignancies at 4 years postsurgery,” she said.
Long-Term Outcomes
After a median follow-up of 4.5 years, the 4-year event-free survival was significantly improved with paclitaxel and carboplatin, with or without veliparib (Table 1).
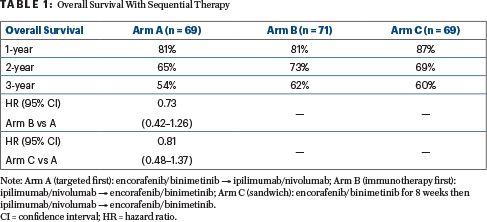
To evaluate the prognostic power of pathologic complete response, the investigators looked at 309 patients with this finding vs 325 without it and found those with a pathologic complete response had a 74% reduction in risk of an event (hazard ratio [HR] = 0.26; P < .0001) compared to those with no pathologic complete response. After a median follow-up of 4.5 years, no significant differences have emerged in overall survival. Deaths have occurred in 12.0% of the paclitaxel/carboplatin/veliparib arm, 10.0% of the paclitaxel/carboplatin arm, and 13.9% of the paclitaxel arm.
Safety Profile
The development of myelodysplastic syndrome, acute myeloid leukemia, and other second primary malignancies was uncommon, and their frequency did not significantly differ among the arms.
“Although there were higher rates of hematologic toxicities with the addition of carboplatin (with or without veliparib), these adverse events did not compromise either treatment delivery or the benefit of carboplatin on the primary endpoint of pathologic complete response or the secondary endpoints of event-free and overall survival,” she said.
DISCLOSURE: Dr. Loibl has received honoraria from Chugai Pharma; has served as an institutional consultant or advisor to AbbVie, Amgen, AstraZeneca/MedImmune, Bayer, Bristol Myers Squibb, Celgene, Daiichi Sankyo, EirGenix, GlaxoSmithKline, Immunomedics, Lilly, Merck KGaA, Novartis, Pfizer, Pierre Fabre, Prime/Medscape, Puma Biotechnology, Roche, Samsung, and Seattle Genetics; has received institutional research funding from AbbVie, Amgen, AstraZeneca, Celgene, Daiichi Sankyo, Immunomedics, Novartis, Pfizer, and Roche; and holds institutional intellectual property in “EP14153692.0.”
REFERENCES
1. Loibl S, Sikov WM, Huober J, et al: Event-free survival, overall survival, and safety of adding veliparib plus carboplatin or carboplatin alone to neoadjuvant chemotherapy in triple-negative breast cancer after ≥ 4 years of follow-up: BrighTNess, a randomized phase 3 trial. ESMO Congress 2021. Abstract 1190. Presented September 17, 2021.
2. Loibl S, O’Shaughnessy J, Untch M, et al: Addition of the PARP inhibitor veliparib plus carboplatin or carboplatin alone to standard neoadjuvant chemotherapy in triple-negative breast cancer (BrighTNess): A randomised, phase 3 trial. Lancet Oncol 19:497-509, 2018.
3. Sikov WM, Berry DA, Perou CM, et al: Impact of the addition of carboplatin and/or bevacizumab to neoadjuvant once-per-week paclitaxel followed by dose-dense doxorubicin and cyclophosphamide on pathologic complete response rates in stage II to III triple-negative breast cancer: CALGB 40603 (Alliance). J Clin Oncol 33:13-21, 2015.
4. von Minckwitz G, Schneeweiss A, Loibl S, et al: Neoadjuvant carboplatin in patients with triple-negative and HER2-positive early breast cancer (GeparSixto; GBG 66): A randomised phase 2 trial. Lancet Oncol 5:747-756, 2014.
5. Loibl S, Weber KE, Timms KE, et al: Survival analysis of carboplatin added to an anthracycline/taxane-based neoadjuvant chemotherapy and HRD score as predictor of response: Final results from GeparSixto. Ann Oncol 29:2341-2347, 2018.

