In the Clinic provides overviews of novel oncology agents, addressing indications, mechanisms, administration recommendations, safety profiles, and other essential information needed for the appropriate clinical use of these drugs.
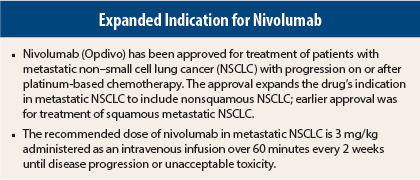
On October 9, 2015, the anti–programmed cell death protein 1 (PD-1) monoclonal antibody nivolumab (Opdivo) was approved for treatment of patients with metastatic non–small cell lung cancer (NSCLC) with progression on or after platinum-based chemotherapy.1,2 The approval expands the indication for nivolumab in metastatic NSCLC to include nonsquamous NSCLC; approval for treatment of squamous metastatic NSCLC in patients with progression on or after platinum treatment was granted in March 2015. Patients with EGFR or ALK alterations should have disease progression on the U.S. Food and Drug Administration–approved therapy for these aberrations prior to receiving nivolumab.
Supporting Efficacy Data
Approval was based on the finding of improved overall survival with nivolumab in a phase III trial in 582 patients with nonsquamous disease comparing nivolumab at 3 mg/kg every 2 weeks (n = 292) vs docetaxel at 75 mg/m2 every 3 weeks (n = 290).2,3 The trial excluded patients with autoimmune disease, medical conditions requiring systemic immunosuppression, symptomatic interstitial lung disease, or untreated brain metastasis.
Overall, patients had a median age of 62 years (37% of nivolumab group and 47% of docetaxel group ≥ 65 years), 55% were male, 92% were white, 12% had previously treated brain metastases, ECOG performance status was 0 in 31% and 1 in 69%, 3.6% had ALK rearrangement, and 14% had EGFR mutation.
Median overall survival was 12.2 months in the nivolumab group vs 9.4 months in the docetaxel group (hazard ratio [HR] = 0.73, P = .0015). The objective response rate was 19% vs 12% (P = .02), and median duration of response was 17 vs 6 months.
There was no significant difference between groups in progression-free survival (median, 2.3 vs 4.2 months, HR = 0.92, P = .39). Evaluation for tumor PD-1 ligand (PD-L1) expression in archived specimens in 78% of patients after study completion showed that 46% were PD-L1–negative (< 1% of cells expressing PD-L1) and 54% of patients were PD-L1–positive (≥ 1% expression). Prespecified subgroup analysis suggested that patients with PD-L1–positive NSCLC had a larger survival treatment effect.
How It Works
Nivolumab is a human immunoglobulin G4 (IgG4) monoclonal antibody that binds the PD-1 receptor on T cells and prevents its interaction with the ligands PD-L1 and PD-L2, thereby blocking PD-1 pathway–mediated inhibition of immune response, including antitumor immune response.
Binding of PD-L1 and PD-L2 to the PD-1 receptor inhibits T-cell proliferation and cytokine production. Upregulation of PD-1 ligands occurs in some tumors, and signaling through this pathway can contribute to inhibition of active T-cell tumor immune surveillance. In syngeneic mouse tumor models, blocking PD-1 activity resulted in decreased tumor growth.
How It Is Used
The recommended dose of nivolumab in metastatic NSCLC is 3 mg/kg administered as an intravenous infusion over 60 minutes every 2 weeks until disease progression or unacceptable toxicity. Infusion should be interrupted or slowed in patients with mild or moderate infusion reactions. Nivolumab should be discontinued for severe or life-threatening infusion reactions.
In patients with metastatic NSCLC, nivolumab treatment should be withheld for grade 2 pneumonitis, grade 2 or 3 diarrhea or colitis, alanine transanimase (ALT) or aspartate transanimase (AST) > 3 to 5 times the upper limit of normal or total bilirubin > 1.5 to 3 times the upper limit of normal, serum creatinine > 1.5 to 6 times the upper limit of normal or > 1.5 times baseline level, grade 2 or 3 hypophysitis, grade 2 adrenal insufficiency, grade 3 rash, encephalitis (new onset moderate or severe neurologic signs or symptoms), and first occurrence of other grade 3 adverse reactions.
There are no recommended dose modifications for hypothyroidism or hyperthyroidism. No dose adjustment is required in patients with renal impairment or mild hepatic impairment; the drug has not been studied in patients with moderate or severe hepatic impairment.
Nivolumab should be discontinued for grade 4 hypophysitis, grade 3 or 4 adrenal insufficiency, grade 4 rash, immune-mediated encephalitis, any life-threatening or grade 4 adverse reaction, grade 3 or 4 pneumonitis, grade 4 diarrhea or colitis, AST or ALT > 5 times the upper limit of normal or total bilirubin > 3 times the upper limit of normal, serum creatinine > 6 times the upper limit of normal, any recurring severe or grade 3 treatment-related adverse reaction, inability to reduce corticosteroid dose to ≤ 10 mg/d of prednisone or equivalent within 12 weeks, and persistent grade 2 or 3 treatment-related adverse reactions that do not recover to grade 0 or 1 within 12 weeks after the last dose.
Safety Profile
In the phase III trial in nonsquamous metastatic NSCLC, the most common adverse events of any grade in the nivolumab group included fatigue/asthenia (49%, grade 3 or 4 in 6%), musculoskeletal pain (36%), cough (30% vs 25% in docetaxel group), decreased appetite (29% vs 22%), and constipation (23% vs 17%); pruritus was more common with nivolumab (11% vs 2%). Pleural effusion was observed in 5.6% and pulmonary embolism in 4.2% of nivolumab patients.
The most common grade 3 or 4 adverse events in the nivolumab group (≥ 2% of patients) were dyspnea, fatigue, pneumonia, pulmonary embolism, pleural effusion, hyperglycemia, respiratory failure, and pain. The most common grade 3 or 4 laboratory abnormalities (≥ 2% of patients) included lymphopenia, hyponatremia (6% vs 2.7%), anemia, increased AST (2.8% vs 0.4%), and increased ALT (2.4% vs 0.4%).
Immune-mediated adverse events occurring in patients receiving nivolumab included hypothyroidism/thyroiditis, rash, pneumonitis, diarrhea/colitis, hyperthyroidism, hepatitis, nephritis, limbic encephalitis, and polymyalgia rheumatica.
Serious adverse events occurred in 47% of nivolumab patients, with the most common (≥ 2% of patients) being pneumonia, pulmonary embolism, dyspnea, pleural effusion, and respiratory failure. Adverse events led to nivolumab delay in 29% of patients and discontinuation in 13%. Among nivolumab patients, there were seven deaths due to infection (including one case of Pneumocystis jirovecii pneumonia), four due to pulmonary embolism, and one due to limbic encephalitis.
Nivolumab carries warnings/precautions for immune-mediated adverse reactions, including immune-mediated pneumonitis, colitis, hepatitis, endocrinopathies (including hypophysitis, adrenal insufficiency, hypothyroidism, and hyperthyroidism), nephritis, renal dysfunction, rash, and encephalitis. It also carries warnings/precautions for embryofetal toxicity.
Patients should be monitored for liver, kidney, thyroid, and neurologic function. Breastfeeding women should discontinue breastfeeding while receiving nivolumab. ■
References
1. U.S. Food and Drug Administration: Nivolumab injection. Available at www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm466576.htm. Accessed October 15, 2015.
2. Opdivo (nivolumab) injection for intravenous use prescribing information, Bristol-Myers Squibb Company, October 2015. Available at www.accessdata.fda.gov/drugsatfda_docs/label/2015/125554s005lbl.pdf. Accessed October 15, 2015.
3. Borghaei H, Paz-Ares L, Horn L, et al: Nivolumab versus docetaxel in advanced nonsquamous non–small-cell lung cancer. N Engl J Med. September 27, 2015 (early release online).