The results of a meta-analysis conducted in the United Kingdom may guide clinicians in the use of docetaxel and bisphosphonates in patients with hormone-sensitive prostate cancer.1
Claire L. Vale, PhD, Senior Research Scientist at the Medical Research Council Clinical Trials Unit at University College London, and colleagues conducted a meta-analysis that examined the overall survival and failure-free survival benefit of both docetaxel and bisphosphonates, added to standard of care, among men with metastatic and nonmetastatic hormone-sensitive disease. She presented the findings at the 2015 European Cancer Congress.
“Results are emerging from randomized controlled trials about adding systemic treatments to standard of care for metastatic and nonmetastatic hormone-sensitive prostate cancer. There is a need to evaluate the accumulating evidence through systematic review, which can guide clinical practice, inform clinical trials, and assess the need for further syntheses of the evidence,” Dr. Vale said.
The aim of the meta-analysis, she said, was to “build a clear picture of all the evidence” pertaining to the addition of docetaxel and bisphosphonates, an area of “immediate interest.”
Outcomes were separately assessed for metastatic and nonmetastatic disease, with the endpoints being overall survival and failure-free survival at 4 years (the time point with most consistent follow-up). Most patients received docetaxel at 75 mg/m2 every 3 weeks for 6 or 9 cycles. Trials had to have sufficient data on these endpoints and reasonable power to show a 5% to 10% benefit.
Docetaxel in the Metastatic Setting
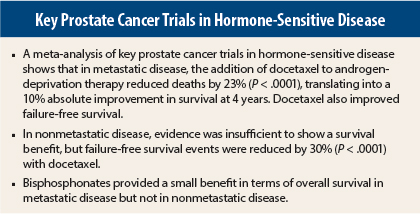
For men with metastatic disease, the addition of docetaxel to standard of care was shown to convey an overall survival benefit, when the results from three trials—CHAARTED, GETUG-15, and STAMPEDE were pooled in a meta-analysis.
The hazard ratio for overall survival was 0.77 (P < .0001), favoring the addition of docetaxel to standard of care. This finding translated into a 10% absolute improvement in survival (from 40% to 50%) at 4 years. Docetaxel also improved failure-free survival, with a hazard ratio of 0.64 (P < .0001), which translated into a 15% absolute reduction in failure (from 80% to 65%).
Docetaxel in Nonmetastatic Disease
In men with nonmetastatic disease, the evidence was insufficient for finding a survival benefit with docetaxel; however, failure-free survival was improved when the findings of four trials—GETUG-12, RTOG 0521, STAMPEDE, and TAX-3501 were pooled.
The hazard ratio for survival was 0.87 (P = .218), translating into a 5% potential improvement in survival (from 80% to 85%) at 4 years. For failure-free survival, the effect was statistically significant, with a hazard ratio of 0.70 (P < .0001), yielding an 8% absolute reduction in failure (from 70% to 62%).
“The hazard ratio of 0.87 for overall survival was not statistically significant, but it suggests a trend toward a survival benefit,” Dr. Vale noted, adding that more data from unreported trials and additional follow-up from the trials included would be vital to obtain a more reliable estimate of the effect of docetaxel on survival in these men.
Bisphosphonates in the Metastatic Setting
“In men with metastatic disease, we found some evidence that adding bisphosphonates to standard of care improves overall survival, but any potential benefit of zoledronic acid is small and not clinically meaningful,” Dr. Vale said.
The findings were based on three trials—CALGB 90202, PR05, and STAMPEDE. Two trials evaluated zoledronic acid at 4 mg every 3 or 4 weeks, whereas one evaluated sodium clodronate at 2,080 mg/d plus standard of care.
The hazard ratio for overall survival when all three trials were pooled in a meta-analysis was 0.88 (P = .025), translating into a 5% absolute improvement in survival (from 40% to 45%) at 4 years. When zoledronic acid was evaluated separately, the hazard ratio was 0.94 (P = .323), translating into a 2.5% potential improvement in survival (from 40% to 42.5%).
“The analysis of the zoledronic acid trials lost some power, and we see a hazard ratio that, while not statistically significant, shows a slight trend favoring zoledronic acid,” noted Dr. Vale, adding that the survival benefit was unlikely to be clinically relevant.
Bisphosphonates in Nonmetastatic Disease
In nonmetastatic disease, no overall survival benefit was observed with the addition of bisphosphonates, based on the pooled analysis of four studies—PR04, RADAR, STAMPEDE, and ZEUS.
The hazard ratio for survival was when the findings of all four trials were pooled was 1.02 (P = .724). With zoledronic acid, the hazard ratio was 0.97 (P = .782), “suggesting no treatment effect in these men,” she said.
Concluding Thoughts
“We think that the reported trials have given us substantial and reliable evidence that adding docetaxel in men with metastatic disease improves both overall survival and failure-free survival and should become the new standard of care for these men, where they are fit and able to take docetaxel,” Dr. Vale said.
In the nonmetastatic setting, the evidence showed that adding docetaxel improves failure-free survival, “but we need more evidence to properly assess overall survival,” she added.
For bisphosphonates, although there is a small survival benefit overall in men with metastatic disease, the potential benefit of zoledronic acid is small and is unlikely to have an impact. In metastatic disease, there is no evidence of a survival improvement with the addition of bisphosphonates; the investigators have not yet assessed their impact on other outcomes. ■
Disclosure: Dr. Vale reported no potential conflicts of interest.
Reference
1. Vale C, Rydzewska LH, Tierney JF, et al: What is the current evidence for adding docetaxel or bisphosphonates to androgen deprivation therapy in men with hormone sensitive prostate cancer? A systematic review and meta-analyses. 2015 European Cancer Congress. Abstract 20LBA. Presented September 27, 2015.