Aromatase inhibitors have demonstrated efficacy in reducing the risk of breast cancer recurrence in hormone receptor–positive patients, but medication compliance can be limited by uncomfortable side effects, including musculoskeletal pain and dysfunction. Musculoskeletal symptoms have been reported in 5% to 61% of patients on aromatase inhibitors,1 with one study demonstrating that 20% of patients may discontinue the drug due to these side effects.2
These symptoms can present as multijoint arthralgias but may also focally affect specific joints, including the small joints of the hands and feet, hips, shoulders, and low back. In addition, patients may develop focal inflammation with edema, causing symptoms such as trigger finger, carpal tunnel syndrome, and De Quervain’s tenosynovitis of the wrist.
Pathophysiology and Diagnosis
The etiology of these symptoms is not completely clear, but there are several theories. One is that estrogen deprivation leads to degradation of joint cartilage and joint inflammation,3 and radiographic studies have demonstrated an increase in joint and tenosynovial fluid in patients on these drugs.4 Another theory is that estrogen may have antinociceptive effects5 and that estrogen deprivation brought on by an aromatase inhibitor may hypersensitize patients to pain.
Patients with preexisting musculoskeletal disorders may be more prone to these side effects, and a pretreatment evaluation can be helpful. Some studies have demonstrated that these symptoms have resulted in an “unmasking” of previously undiagnosed rheumatologic disorders,6 potentially necessitating that a preexisting rheumatologic disorder is ruled out prior to treatment initiation.
Diagnostic criteria for aromatase inhibitor–induced musculoskeletal symptoms have been published but not validated. One suggested criterion is that the patient must have musculoskeletal symptoms that start while on the medication, improve within 2 weeks of stopping the medication, and restart when the aromatase inhibitor is resumed again.7 However, further research is needed to identify and validate appropriate criteria for diagnosis.
Treatment and Its Side Effects
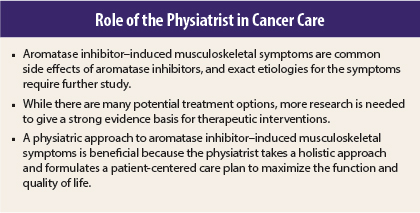
To date, there is a dearth of high-quality research into therapeutic interventions for these symptoms. A physiatric approach will take into account all of the patient’s physical symptoms and how they impact his or her function, using a biopsychosocial model. In addition, it may be helpful to talk to patients about their attitude toward the aromatase inhibitor, as some patients strongly consider discontinuing the medication due to its side effects. Other patients may report that they would never consider discontinuation, regardless of side effects.
A sensible approach to the management of musculoskeletal side effects is to provide a global approach that will improve symptoms in multiple body regions as well as a focused approach on particularly symptomatic areas. As a more global approach, exercise has been studied to improve musculoskeletal symptoms, with a recent study looking at 150 minutes per week of moderate-intensity cardiovascular exercise and 2 days a week of resistance training, showing a statistically significant improvement in pain scores in patients on aromatase inhibitors.8
Medications could also be considered for these symptoms, although, again, research is lacking on what is appropriate. Common pain medications such as acetaminophen, topical or oral nonsteroidal anti-inflammatory drugs, tramadol, or opioids, should be considered although there is little available evidence-based literature on these treatments.
A single-arm trial of duloxetine—up to 120 mg/d— showed clinically significant improvement in pain scores in patients on aromatase inhibitors.9 Glucosamine (1,500 mg/d) and chondroitin sulfate (1,200 mg/d) showed moderate improvement in musculoskeletal symptoms after 24 weeks of treatment.10
Vitamin D levels may or may not be significant contributors to aromatase inhibitor–induced musculoskeletal symptoms, as studies have been conflicting.11,12 Acupuncture has also been studied with mixed results.13,14
For focal symptoms, different approaches can be considered. If there is a particularly symptomatic joint or region, physical or occupational therapy can be considered for pain reduction, range of motion, and joint protection. Physiatric management is helpful, as other interventions such as bracing of the joint or therapeutic injections with corticosteroid or hyaluronic acid (for the knee) can be utilized. In my clinical practice, periodic joint injections for the most symptomatic region(s) have been a very helpful adjunct to other treatments for moderate to severe pain.
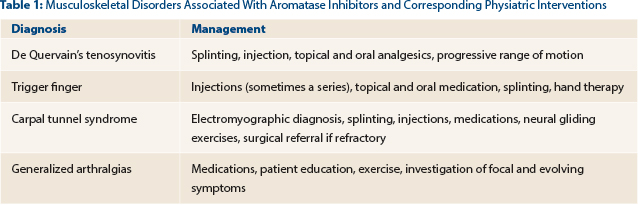
Given how common wrist and hand pain is in patients on aromatase inhibitors, correct diagnosis of the etiology of this pain is essential. Physiatric workup and management of wrist pain (including carpal tunnel syndrome, De Quervain’s tenosynovitis, and carpometacarpal osteoarthritis) and trigger finger can optimize patient care. Examples of musculoskeletal disorders attributable to aromatase inhibitors and their respective physiatric interventions are listed in Table 1.
As a last resort, a permanent or temporary holiday from the aromatase inhibitor could be considered. Alternatively, switching to a different aromatase inhibitor, or even tamoxifen, may be beneficial. Consideration of this option should involve a discussion between the patient and her oncologist about the risks and benefits of such a decision.
Providing Patient Encouragement
Finally, patient encouragement can be helpful. It helps when a patient’s symptoms are validated. Patients may feel frustrated if their physicians minimize the side effects of hormone therapy. Likewise, they may feel relieved to know that this is a potentially normal experience while on these drugs and that symptoms should subside after the course of hormone therapy is completed (depending on the necessary duration of treatment).
In addition, some data suggest that aromatase inhibitor–induced musculoskeletal symptoms may be associated with a survival benefit,15 which obviously could be heartening to the patient. Patients often feel encouraged when coming to see a physiatrist and learning that there are solutions to help relieve their symptoms. As a result, they may be more willing to “ride out” their treatment side effects. ■
Disclosure: Dr. Wisotzky reported no potential conflicts of interest
References
1. Gaillard S, Stearns V: Aromatase inhibitor-associated bone and musculoskeletal effects: New evidence defining etiology and strategies for management. Breast Cancer Res 13:205, 2011.
2. Presant CA, Bosserman L, Young T, et al: Aromatase inhibitor-associated arthralgia and/or bone pain: Frequency and characterization in non-clinical trial patients. Clin Breast Cancer 7:775-778, 2007.
3. Tsai CL, Liu TK, Chen TJ: Estrogen and osteoarthritis: A study of synovial estradiol and estradiol receptor binding in human osteoarthritic knees. Biochem Biophys Res Commun 183:1287-1291, 1992.
4. Lintermans A, Laenen A, Van Calster B, et al: Prospective study to assess fluid accumulation and tenosynovial changes in the aromatase inhibitor-induced musculoskeletal syndrome: 2-year follow-up data. Ann Oncol 24:350-355, 2013.
5. Felson DT, Cummings SR: Aromatase inhibitors and the syndrome of arthralgias with estrogen deprivation. Arthritis Rheum 52:2595-2598, 2005.
6. Shanmugam VK, McCloskey J, Elston B, et al: The CIRAS study: A case control study to define the clinical, immunologic, and radiographic features of aromatase inhibitor-induce musculoskeletal symptoms. Breast Cancer Res Treat 131:699-708, 2012.
7. Nivavath P: Aromatase inhibitor-induced arthralgia: A review. Ann Oncol 24:1443-1449, 2013.
8. Irwin ML, Cartmel B, Gross C, et al: Randomized exercise trial of aromatase inhibitor-induced arthralgia in breast cancer survivors. J Clin Oncol 33:1104-1111, 2015.
9. Henry NL, Banerjee M, Wicha M, et al: Pilot study of duloxetine for treatment of aromatase inhibitor-associated musculoskeletal symptoms. Cancer 117:5469-5475, 2011.
10. Greenlee H, Crew KD, Shao T, et al: Phase II study of glucosamine with chondroitin on aromatase inhibitor-associated joint symptoms in women with breast cancer. Support Care Cancer 21:1077-1087, 2013.
11. Khan QJ, Reddy PS, Kimler BF, et al: Effect of vitamin D supplementation on serum 25-hydroxy vitamin D levels, joint pain, and fatigue in women starting adjuvant letrozole treatment for breast cancer. Breast Cancer Res Treat 119:111-118, 2010.
12. Singh S, Cuzick J, Mesher D, et al: Effect of baseline serum vitamin D levels on aromatase inhibitors induced musculoskeletal symptoms: Results from the IBIS-II, chemoprevention study using anastrozole. Breast Cancer Res Treat 132:625-629, 2012.
13. Crew KD, Capodice JL, Greenlee H, et al: Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor-associated joint symptoms in women. J Clin Oncol 28:1154-1160, 2010.
14. Bao T, Cai L, Giles JT, et al: A dual-center randomized controlled double blind trial assessing the effect of acupucture in reducing musculoskeletal symptoms in breast cancer patients taking aromatase inhibitors. Breast Cancer Res Treat 138:167-174, 2013.
15. Fontein DB, Seynaeve C, Hadji P, et al: Specific adverse events predict survival benefit in patients treated with tamoxifen or aromatase inhibitors: An international tamoxifen exemestane adjuvant multinational trial analysis. J Clin Oncol 31:2257-2264, 2013.
GUEST EDITOR
Physiatry in Oncology explores the benefits of cancer rehabilitation in oncology clinical practice to screen survivors for physical and cognitive impairments along the care continuum to minimize survivors’ disability and maximize their quality of life. The column is guest edited and occasionally written by Sean Smith, MD, Director of the Cancer Rehabilitation Program at the University of Michigan Department of Physical Medicine and Rehabilitation in Ann Arbor.