Molecular categorization of tumors with immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH) has become a critical component in the diagnosis and treatment of breast cancer, improving outcomes by assigning the most appropriate therapy to specific tumor pathways. According to a study presented at the 2015 Breast Cancer Symposium, a new functional molecular subtyping reclassifies approximately 23% of tumors compared to conventional immunostaining, with potential therapeutic and prognostic implications.1
“BluePrint 80-gene subtyping yielded significantly better correlation with both neoadjuvant chemotherapy responsiveness in the HER2-positive group and basal group, as well as resistance—putting more people into the luminal group, which is fairly resistant to chemotherapy,” said Peter D. Beitsch, MD, Director of the Dallas Breast Center. “The 80-gene subtyping divided triple-positive [HER2-positive/hormone receptor–positive] cancers into two groups of almost equal size: one being luminal-driven and one being HER2/neu-driven.”
He added, “This triple-positive/80-gene luminal subtype is relatively resistant to neoadjuvant chemotherapy with trastuzumab [Herceptin] alone, however pertuzumab [Perjeta] overcame resistance to chemotherapy/trastuzumab in a substantial portion of the triple-positive/80-gene luminal subtype.”
Neoadjuvant Breast Symphony Trial
As Dr. Beitsch noted, classification into molecular subtypes is important for the selection of therapy for patients with breast cancer, as previous analyses have demonstrated that these subtypes have distinct clinical outcomes.
The primary aim of the Neoadjuvant Breast Symphony Trial (NBRST) was to compare a multigene classifier to conventional IHC/FISH subtyping to predict chemosensitivity as defined by pathologic complete response.
Researchers enrolled 1.000 patients from 62 U.S. institutions and reported on 889 who have completed all therapy. The median age of the cohort was 52. Over 90% of the patients had stage II or III disease. Two-thirds of patients had hormone receptor–positive breast cancer, 23% had triple-negative disease, and 29% were HER2-positive.
The 80-gene assay split tumors into luminal-type, HER2/neu-type, and basal-type. The 70-gene assay further divided luminal type into luminal A and luminal B. All of the assays were completed on a core biopsy upfront.
“Patients received neoadjuvant chemotherapy or systemic endocrine therapy based on [National Comprehensive Cancer Network] guidelines. Patients then came to surgery. Pathology was reported as either complete or partial response to neoadjuvant chemotherapy .
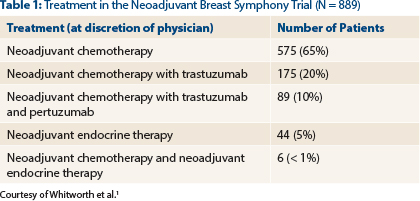
“A few patients received neoadjuvant endocrine therapy, but that was only 5% of the whole group,” he observed, “but we are reporting only on the neoadjuvant chemotherapy patients [see Table 1].”
Patients who were classified as HER2-positive received HER2-directed therapy, which changed from trastuzumab alone to trastuzumab plus pertuzumab, as standard of care in the middle of the trial.
Key Results
Compared to conventional IHC and FISH subtyping, the 80-gene functional subtyping reclassified more than 1 in 5 tumors. Approximately 20% of the original luminal group were reclassified into the basal group. These were all estrogen receptor–positive tumors with > 50% having > 10% positivity.
“We increased the basal group by 50% with molecular subtyping compared to immunostaining, but we maintained [pathologic complete response] rates in that group,” said Dr. Beitsch.
The original basal group and the HER2-positive/hormone receptor–negative group basically remained the same, he noted. The group with the biggest change, however, was the triple-positive group (estrogen receptor–positive, progesterone receptor–positive, and HER2-positive), where half the patients had HER2-driven disease and the HER2 subtype and half had the luminal subtype.
“When we reclassified patients into ‘proper subtypes,’” said Dr. Beitsch, “the number of patients [with HER2-driven disease] went down from 258 to 141, but the [pathologic complete response] rate actually increased considerably and was statistically significant compared to surrogate immunohistochemical subtyping.”
Problem Solved
As Dr. Beitsch explained, the conundrum of patients with triple-positive disease having less responsiveness to trastuzumab and chemotherapy has been well documented for years. When reclassified by functional subtyping, however, the group that was classified as HER2-driven had nearly a 50% pathologic complete response rate. Conversely, patients with triple-positive disease who were molecularly subtyped into the luminal group were basically nonresponsive to neoadjuvant chemotherapy plus trastuzumab alone.
“We solved the problem with triple-positive patients,” said Dr. Beitsch. “They’re actually two subtypes of equal numbers in the groups, but their response rates are remarkably different.”
However, during the course of the trial, Dr. Beitsch observed a marked increase in pathologic complete response in this previously unresponsive group.
When we looked at this group of triple-positive luminal patients, their [pathologic complete response] rate went from 3% to 18%. We then noticed that standard of care changed in the middle of the trial, when we went from chemotherapy plus trastuzumab to chemotherapy plus trastuzumab plus pertuzumab. This change corresponded exactly with the increase in pathologic complete response, which in fact had increased 10-fold! ■
Disclosure: Dr. Beitsch is a member of the speakers bureau for and has received research funding from Agendia.
Reference
1. Whitworth PW, Beitsch PD, Rotkis MC, et al: Functional subtyping with BluePrint 80-gene profile to identify distinct triple-positive subtypes with and without trastuzumab/chemosensitivity. 2015 Breast Cancer Symposium. Abstract 114. Presented September 25, 2015.