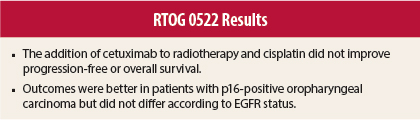
Use of cisplatin or cetuximab (Erbitux) with radiotherapy improves overall survival in stage III or IV head and neck carcinoma, and adding cetuximab to platinum therapy improves overall survival in metastatic disease. In the phase III Radiation Therapy Oncology Group (RTOG) 0522 trial reported in the Journal of Clinical Oncology, K. Kian Ang, MD, PhD (now deceased), of The University of Texas MD Anderson Cancer Center, Houston, and colleagues found no progression-free survival or overall survival benefit of adding cetuximab to radiation/cisplatin in stage III or IV disease.1
Rita S. Axelrod, MD, of Thomas Jefferson University Hospital, Philadelphia, is the corresponding author for the Journal of Clinical Oncology article.
Study Details
In the trial, 891 patients with squamous cell carcinoma of the oropharynx, hypopharynx, or larynx and Zubrod performance status 0 or 1 were randomly assigned between November 2005 and May 2009 to receive accelerated radiotherapy plus cisplatin with (n = 444) or without cetuximab (n = 447). Randomization was stratified by tumor site, nodal stage, Zubrod performance status, use of intensity-modulated radiotherapy (IMRT), and use of pretreatment positron-emission tomography/computed tomography scans.
Accelerated radiotherapy included two schedules; in one, 72 Gy was delivered in 42 fractions given over 6 weeks. This included 1.8 Gy/fraction per day for 5 days per week and 1.5 Gy/fraction as a second daily treatment for the last 12 treatment days. When IMRT was used, the schedule included 70 Gy in 35 fractions (2 Gy per fraction), with twice-daily dosing once a week for 5 weeks. Cisplatin was given at 100 mg/m2 on days 1 and 22 of radiotherapy, and cetuximab was given at 400 mg/m2 the week before radiotherapy and then 250 mg/m2 per week during radiotherapy. The primary endpoint was progression-free survival in the intention-to-treat population.
The cetuximab and control groups were generally balanced for age (median, 58 and 57 years), sex (90% and 87% male), race (90% and 92% white), Zubrod performance status (0 in 66% and 65%), primary tumor site (oropharynx in 70% in both, hypopharynx in 7% in both, larynx in 23% in both), T category (T2 in 40% and 39%, T3 in 36% and 38%, T4 in 24% and 23%), N category (eg, N0 in 12% and 10%, N2b in 35% and 31%, N2c in 31% and 36%), stage (IV in 85% and 87%), p16-positive primary oropharyngeal tumor (39% and 36%, unknown in 47% and 50%), and EGFR status (27% and 26% with < 80% positive tumor cells, 16% in both with ≥ 80% positive tumor cells, unknown in 57% in both).
No Survival Difference
Median follow-up was 3.8 years. There were no significant differences between the cetuximab and control groups in 30-day mortality (2.0% vs 1.8%, P = .81) or in 3-year progression-free survival (58.9% vs 61.2%, hazard ratio [HR] = 1.08, P = .76), overall survival (75.8% vs 72.9%, HR = 0.95, P = .32), locoregional failure (25.9% vs 19.9%, HR = 1.30, P = .97), or distant metastasis (9.7% vs 13.0%, HR = 0.76, P = .08). On subgroup analysis, an overall survival benefit of cetuximab was observed in patients aged ≤ 50 years (HR = 0.45, P = .02 for interaction), with the addition of cetuximab not appearing to affect outcome in other subgroups.
Trends for a differential effect of cetuximab according to p16 status were observed; hazard ratios were 1.57 for p16-positive disease and 0.86 for p16-negative disease for progression-free survival (P = .12 for interaction) and 1.42 and 0.69, respectively, for overall survival (P = .13 for interaction). After imputation and adjustment for prognostic factors, hazard ratios were reduced to 1.29 and 0.92 for progression-free survival (P = .31 for interaction) and 1.10 and 0.63 for overall survival (P = .19 for interaction).
On multivariate analysis, primary laryngeal-hypopharyngeal carcinoma, p16-negative oropharyngeal cancer, N2b-3 category, T4 tumor, > 10 pack-years smoking history, age > 50 years, and Zubrod performance status of 1 were significantly associated with poorer progression-free and overall survival.
Effect of p16 and EGFR Status
Among all patients, those with p16-positive vs p16-negative oropharyngeal carcinoma had significantly better 3-year progression-free survival (72.8% vs 49.2%, HR = 0.49, P < .001), overall survival (85.6% vs 60.1%, HR = 0.32, P < .001), locoregional failure (HR = 0.45, P < .001), and distant metastasis (HR = 0.37, P = .005). Epidermal growth factor receptor (EGFR) expression ≥ 80% vs < 80% was not associated with 3-year progression-free survival (HR = 1.09, P = .60), overall survival (HR = 1.19, P = .37), locoregional failure (HR = 0.93, P = .76), or distant metastasis (HR = 1.53, P = .14).
Toxicity
Grade 3 or 4 acute toxicities that were more common (all P < .05) in the cetuximab group included radiation mucositis (43% vs 33%), skin reaction outside portal (20% vs 1%), skin reaction inside portal (25% vs 15%), fatigue (14% vs 9%), anorexia (16% vs 11%), and hypokalemia (10% vs 5%). However, late grade 3 or 4 toxicities (> 90 days from start of radiotherapy) were not observed more frequently in the cetuximab group.
More treatment-related grade 5 adverse events occurred in the cetuximab group (10 vs 3, P = .05). The cetuximab group was more likely to have interruption of radiotherapy (26.9% vs 15.1%).
For the cetuximab vs control groups, rates of feeding tube dependency were 18.8% vs 21.2% at 1 year (P = .47), 11.9% vs 13.5% at 2 years (P = .56), and 7.0% vs 12.1% at 3 years (P = .05).
The investigators concluded: “Adding cetuximab to radiation-cisplatin did not improve outcome and hence should not be prescribed routinely. [Progression-free and overall survival] were higher in patients with p16-positive [oropharyngeal carcinoma], but outcomes did not differ by EGFR expression.” ■
Disclosure: The study was supported by grants from the National Cancer Institute. For full disclosures of the study authors, visit jco.ascopubs.org.
Reference
1. Ang KK, Zhang Q, Rosenthal DI, et al: Randomized phase III trial of concurrent accelerated radiation plus cisplatin with or without cetuximab for stage III to IV head and neck carcinoma: RTOG 0522. J Clin Oncol. August 25, 2014 (early release online).