High-risk atypical benign breast lesions are upgraded to cancer in more than 15% of patients, but the routine excision of such lesions is probably unnecessary. At the 2014 Breast Cancer Symposium in San Francisco, researchers presented information that could guide the selection of patients who might safely avoid surgery.1
Alvaro Peña, MD, and colleagues from the Mayo Clinic, Rochester, Minnesota, evaluated clinical, imaging, and histologic features associated with cancer upgrade in cases with atypical ductal hyperplasia in a core needle biopsy and developed a multivariate model to predict this risk. The model was based on a retrospective review of patients undergoing surgical excision of atypical ductal hyperplasia diagnosed by core biopsy between 2005 and 2013 at the Mayo Clinic.
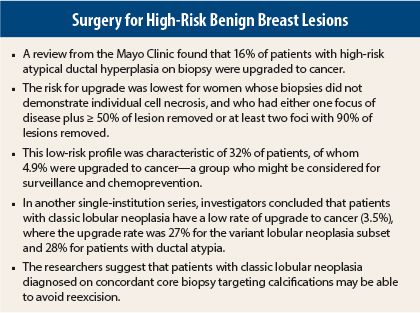
Of 399 biopsies, 55 were found to be ductal carcinoma in situ and 9 were invasive cancers. These 64 lesions yielded an upgrade rate of 16%.
In the multivariate analysis, three factors related to core biopsy were strongly associated with upgrade: the estimated percentage of lesion removed by imaging, presence of individual cell necrosis, and number of foci of atypical ductal hyperplasia. Their prediction model showed an average C-statistic (ie, the area under the receiver operating characteristic curve) of 0.77, and was based on the following odds ratios (ORs):
- Percentage of lesion removed: with the reference being > 90% removed, risk was highest among patients with < 50% removed (OR = 3.8) and was moderate (OR = 1.4) for those with 50% to 90% removed (P < .001).
- Presence of individual cell necrosis: compared to patients without necrosis, upgrade was more likely when biopsies showed individual cell necrosis (OR = 4.3, P < .001).
- Number of foci of atypical ductal hyperplasia: compared to patients with just one focus, upgrade was more likely among patients with two or three foci (OR = 2.1) and more than three foci (OR = 3.6, P = .009).
The predictive model showed a subgroup with low risk for upgrade at excision: women with (1) no individual cell necrosis, and (2) either one focus with ≥ 50% removal, or two to three foci with 90% removal. Approximately 32% of the sample met these criteria and 4.9% were upgraded to cancer. In contrast, those not meeting this had an upgrade rate of 21.4%.
“If these findings are validated, women whose biopsies meet low-risk criteria might be considered for prevention therapy and surveillance rather than surgical excision,” Dr. Peña suggested.
Lobular Neoplasia: Can Some Patients Avoid Surgery?
Investigators from Virginia Piper Cancer Institute in Minneapolis, Minnesota, evaluated the need for reexcision among patients with lobular neoplasia diagnosed on core biopsy. Their study aimed to determine the “upgrade” rates in these patients and to identify subsets of those who do not require subsequent surgical excision. The study was presented by Barbara Susnik, MD.2
The analysis was based on 13,772 breast core biopsies, of which 373 cases (2.7%) were lobular neoplasia. A final cohort of 302 patients underwent 316 biopsies that revealed classic lobular neoplasia (n = 228), lobular neoplasia with ductal atypia (n = 53), and variant lobular neoplasia (n = 15), including lobular carcinoma in situ with necrosis and pleomorphic lobular carcinoma in situ.
In patients with pure lobular neoplasia, 20 patients had a synchronous ipsilateral core biopsy containing cancer. Of these, biopsy sites closely approximated the same quadrant in five patients, and two biopsy sites were in different quadrants in 15 patients. Discordance between imaging and pathologic assessments was observed in six cases (2.6%).
In the classic lobular neoplasia group, eight patients (3.5%) were upgraded to carcinoma (ductal carcinoma in situ in five and invasive cancer in three). Seven of these patients were biopsied for calcification. The researchers found no association between upgrade and high risk (ie, family or personal history), type of pure lobular neoplasia in the core biopsy, calcifications in the core biopsy, and size of targeted calcifications.
In contrast, in the variant group, four (27%) were upgraded, and in the subset with lobular neoplasia with ductal atypia, 15 (28%) were upgraded.
“While lobular neoplasia with nonclassic morphology or with associated ductal atypia requires surgical excision, this can be avoided in classic lobular neoplasia diagnosed on core biopsy,” Dr. Susnik suggested.
She advised that pathologists as well as radiologists should correlate imaging findings with pathology, and radiologists must critically evaluate the targeted calcifications to assure the lesion has been adequately sampled.
These findings led the researchers to recommend surgical excision for patients with:
- lobular neoplasia on core biopsy with discordant findings
- lobular neoplasia variants (lobular carcinoma in situ with necrosis, pleomorphic lobular carcinoma in situ)
- lobular neoplasia associated with another risk lesion (such as atypical ductal hyperplasia and flat epithelial atypia)
- lobular neoplasia when the imaging target is mass/density/asymmetry on magnetic resonance imaging
Based on difficulties in assessing upgrade, excision should also be considered for patients having synchronous biopsy with carcinoma in the same breast. ■
Disclosure: Drs. Peña and Susnik reported no potential conflicts of interest.
References
1. Peña A, Fazzio RT, Shah S, et al: A multivariate model to predict cancer upgrade from atypical ductal hyperplasia by core needle biopsy. Breast Cancer Symposium. Abstract 3. Presented September 5, 2014.
2. Susnik B, Day D, Krueger J, et al: Surgical outcome of lobular neoplasia diagnosed in core biopsy: Prospective study of 316 cases. Breast Cancer Symposium. Abstract 4. Presented September 5, 2014.