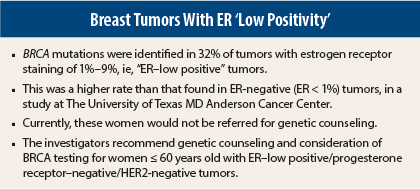
BRCA mutations may occur in nearly one-third of breast cancer patients who would have been described as having triple-negative cancer except that their tumors express low levels of estrogen receptor, so the tumors are described as ER–low positive, according to researchers from The University of Texas MD Anderson Cancer Center, Houston, who presented their findings at the 2014 Breast Cancer Symposium in San Francisco.1
“The rate of deleterious BRCA1/2 germline mutations in ER-negative vs ER–low positive (1%–9%) breast cancer is similar,” reported Rachel Ann Sanford, MD, a medical oncology fellow at MD Anderson. The reported incidence of deleterious germline BRCA mutations in patients with triple-negative tumors is 11% to 24%.
The investigators are recommending, therefore, that BRCA testing be offered not just to women under age 60 with tumors that are ER/progesterone receptor–negative and HER2-negative, but also to those with tumors that are ER–low positive.
The 2011 guidelines from ASCO and the College of American Pathologists recommend that breast cancers with estrogen receptor staining as low as 1% on immunohistochemistry be considered ER-positive. This means that guidelines for referring patients to genetic counseling and possible BRCA testing—ie, those under the age of 60 with triple-negative breast cancer—exclude patients with ER–low positive tumors (those staining at 1% to 9%).
“This may lead to the undertesting of appropriate patients,” Banu Arun, MD, the senior investigator, said in an interview with The ASCO Post. Dr. Arun is Professor of Breast Medical Oncology and Co-Director of the Clinical Cancer Genetics program at MD Anderson.
“We still need to test these patients. In our study, 1% to 9% of
ER-positive patients had BRCA mutation rates similar to triple-negative patients. And it is thought that biologically these tumors act more like triple-negative tumors,” she said.
Study Details
Their study was a review of a prospectively maintained research database of all breast cancer patients seen at MD Anderson between 2004 and 2014. Of these, 1,608 had tumors with estrogen receptor staining < 10% and negative progesterone receptor and HER2 status. BRCA testing results were obtained for 144 of these patients. Most had been referred for genetic counseling because of family history, Dr. Sanford noted.
There were 22 patients with ER staining of 1% to 9%, and of these, 7 (31.8%) tested positive for a deleterious BRCA germline mutation. This was BRCA1 in 22.7% and BRCA2 in 9.1%. Of the 122 patients with ER < 1% (ie, labeled as ER-negative), 33 patients (27%) had BRCA mutations.
“The incidence of deleterious germline BRCA mutations in patients with ER–low positive vs ER-negative breast cancers is not significantly different,” Dr. Sanford reported. “Therefore, we strongly recommend that BRCA testing be offered to women under age 60 with tumors that are ER–low positive, in addition to those that are progesterone receptor–negative and HER2-negative.”
The researchers acknowledged that this study was based on a small population of patients who may not be representative of typical breast cancer patients. They would like to validate the findings in larger, more diverse populations to produce “more robust data” that might facilitate a change in the current guideline, Dr. Arun said.
Interest From the Audience
Stuart J. Schnitt, MD, Professor of Pathology at Harvard Medical School, Boston, found the research provocative and said it clearly has clinical ramifications.
“The issue of what constitutes an ER-positive tumor is a huge clinical problem. I can’t tell you how many cases I have seen that under the microscope look basal-like, and when I pick up the ER stain, I am hoping I don’t find ER positivity in the 1% range. I don’t think we are doing these patients a favor by calling them ER-positive,” Dr. Schnitt offered during the discussion.
He said that molecular studies have shown that some of these tumors cluster in basal-like groups and have characteristics that are not compatible with ER-positive tumors. “It’s almost like these are the ER equivalent to HER2 2+ tumors,” he suggested. “I almost wonder if we need to find out if they are functionally ER-positive or really triple-negative. The good thing is, they constitute a relatively small proportion of patients.”
Hope S. Rugo, MD, Professor of Medicine and Director of the Breast Oncology Clinical Trials Program at the University of California, San Francisco, Helen Diller Family Comprehensive Cancer Center, also commented. “This is a small study, but it’s quite an interesting set of data. If this were a clinical trial, we would say the findings are ‘hypothesis-generating’ and warrant further study,” she said. “In the setting of something that can have such a huge impact as finding a BRCA mutation, it’s worth considering screening patients with tumors that look triple-negative but have very low ER positivity.” ■
Disclosure: Dr. Arun reported no potential conflicts of interest. Dr. Rugo receives research funding to UCSF from Novartis, Pfizer, and Lily.
Reference
1. Sanford RA, Song J, Guiterrez-Barrera AM, et al: High incidence of germline BRCA mutation in patients with ER low positive/PR negative/HER2-neu negative tumors. Breast Cancer Symposium. Abstract 2. Presented September 4, 2014.