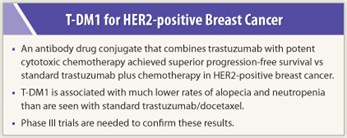
The investigational antibody-drug conjugate T-DM1 improved progression-free survival over standard chemotherapy with docetaxel plus trastuzumab (Herceptin) when given as first-line treatment of HER2-positive metastatic breast cancer, according to an open-label phase II study reported at the 2011 European Multidisciplinary Cancer Congress.1 In addition, T-DM1 was associated with much lower rates of neutropenia and alopecia, which are troubling side effects of standard docetaxel/trastuzumab.
 T-DM1 is a unique agent that combines the monoclonal antibody trastuzumab with a potent cytotoxic chemotherapy (a derivative of maytansine) through a stable linker. When trastuzumab binds to extracellular HER2, the trastuzumab exerts its antitumor benefits and then the entire T-DM1 molecule is taken up into the cell, where the linker releases the potent chemotherapy. To give some idea of its potency, emtansine is 100 times more potent than vincristine in vitro.
T-DM1 is a unique agent that combines the monoclonal antibody trastuzumab with a potent cytotoxic chemotherapy (a derivative of maytansine) through a stable linker. When trastuzumab binds to extracellular HER2, the trastuzumab exerts its antitumor benefits and then the entire T-DM1 molecule is taken up into the cell, where the linker releases the potent chemotherapy. To give some idea of its potency, emtansine is 100 times more potent than vincristine in vitro.
“The stable linker is the magic. I tell my patients that trastuzumab is like a well-aimed gun, and the bullet is the chemotherapy attached,” said Sara Hurvitz, MD, Director of Breast Oncology at the University of California, Los Angeles.
Progression-free survival was significantly improved by T-DM1: a median of 14.2 months vs 9.2 months for standard chemotherapy (P = .0353).
“Patients with metastatic breast cancer who received T-DM1 had a 41% improvement in the time they lived with no worsening of disease compared with standard chemotherapy plus trastuzumab. These provocative data illustrate that first-line treatment with T-DM1 extends time living without cancer with far fewer side effects than standard chemotherapy plus trastuzumab,” Dr. Hurvitz commented.
Unique Agent
“I believe that this is the magic and clever drug we have been waiting for, but we will need validation in a large randomized trial,” said formal discussant Martine Piccart, MD, Institut Jules Bordet, Brussels, Belgium, and President-Elect of the European Society for Medical Oncology.
The study enrolled 137 patients with HER2-positive advanced breast cancer and randomly assigned them to trastuzumab/docetaxel vs T-DM1. Crossover from the control arm to the T-DM1 arm was allowed at disease progression, but the data Dr. Hurvitz presented were pre-crossover. Overall survival data are not mature and will be presented in 2012, and quality-of-life data from the study will be presented at the San Antonio Breast Cancer Symposium in December.
Toxicities and Responses
 At the time of data cutoff, 43.3% of patients in the T-DM1 arm and 21% of controls were on therapy. Median duration of treatment was 10 months with T-DM1 vs 5.5 months for docetaxel. Dr. Hurvitz suggested that the ability to stay on T-DM1 longer may be related to its more favorable toxicity profile.
At the time of data cutoff, 43.3% of patients in the T-DM1 arm and 21% of controls were on therapy. Median duration of treatment was 10 months with T-DM1 vs 5.5 months for docetaxel. Dr. Hurvitz suggested that the ability to stay on T-DM1 longer may be related to its more favorable toxicity profile.
Grades 3 and 4 adverse events were reported in 46% of T-DM1 patients vs 89.4% of controls. Adverse events leading to discontinuation were: 7.2% vs 29%, respectively. More grade 3 or higher neutropenia (6% for T-DM1 vs 61% for controls) and hemorrhagic events (8% vs 17%, respectively) were reported with standard chemotherapy; more grade 1/2 thrombocytopenia occurred with T-DM1: 30% vs 6.1%, respectively.
The rates of nonhematologic toxicities (alopecia, diarrhea, and peripheral edema) were much higher with standard chemotherapy. Only 4% of those who received T-DM1 had alopecia vs 67% of those on the control arm. No significant cardiac events were reported.
Overall response rates were similar between the two arms: 64% for T-DM1 vs 58% for controls. Clinical benefit was reported in 75% of T-DM1 patients vs 81% of controls. The two treatments differed with respect to median duration of response: not yet reached for T-DM1 and 9.5 months for controls.
T-DM1 is being studied in HER2-positive metastatic breast cancer in a comprehensive phase III program. The EMILIA study will compare T-DM1 vs lapatinib (Tykerb) plus capecitabine (Xeloda) in 980 patients; the MARIANNE study will compare docetaxel/trastuzumab vs T-DM1 vs T-DM1 plus pertuzumab; and the TH3RESA study is comparing T-DM1 vs best supportive care in the salvage setting. ■
Disclosure: Dr. Hurvitz has received research grants from Genentech/Roche and a travel grant for symposium travel from Roche. Dr. Piccart receives consultancy fees from Roche, and her institute receives research grants from Roche.
Expert Point of View: European Perspective
Expert Point of View: U.S. Perspective
Reference
1. Hurvitz S, Dirix L, Kocsis J, et al: Trastuzumab emtansine (T-DM1) vs trastuzumab plus docetaxel in previously untreated HER2-positive metastatic breast cancer: Primary results of a randomized, multicenter, open-label, phase II study (TDM4450g/BO21976). 2011 European Multidisciplinary Cancer Congress. Abstract 5001. Presented September 25, 2011.

 Martine Piccart, MD, of the Institut Jules Bordet, Brussels, Belgium, and President-Elect of the European Society for Medical Oncology, was highly enthusiastic about the findings of the phase II T-DM1 study, but said, “We have to remember this is an open-label trial, and in a study like this,...
Martine Piccart, MD, of the Institut Jules Bordet, Brussels, Belgium, and President-Elect of the European Society for Medical Oncology, was highly enthusiastic about the findings of the phase II T-DM1 study, but said, “We have to remember this is an open-label trial, and in a study like this,... “This is an exciting drug,” said Hope Rugo, MD, Professor of Medicine at University of California, San Francisco. “It is highly effective and extremely well tolerated, with no hair loss, which is very important to patients. It also enables using a lower dose of trastuzumab.”
“This is an exciting drug,” said Hope Rugo, MD, Professor of Medicine at University of California, San Francisco. “It is highly effective and extremely well tolerated, with no hair loss, which is very important to patients. It also enables using a lower dose of trastuzumab.”