Specialized exercise and wellness programs significantly elevated physical well-being and quality of life among patients with breast cancer while reducing the use of health-care resources in new research presented at the 2023 American Society of Breast Surgeons Annual Meeting.
In one multicenter study, patients enrolled in an individualized exercise program after surgery scored significantly higher on all quality-of-life measures compared with the control group.1 In turn, these scores were significant predictors of health-care resource utilization, according to Karen Wonders, PhD, Professor of Exercise Physiology and Program Director of Exercise Science at Wright State University in Ohio and Founder and Chief Executive Officer of Maple Tree Cancer Alliance.

Karen Wonders, PhD

Frances Wright, MD
In a second study, Canadian investigators broke new ground in examining the impact of prehabilitation—a program focused on optimizing health during the preoperative period, in this case, neoadjuvant chemotherapy—for patients with breast cancer.2 Although the main aim was to assess feasibility, the study also yielded significant data on the program’s benefits, showing a positive impact on physical fitness and a variety of well-recognized health-related measurements, both at the completion of neoadjuvant treatment and 6 months postoperatively, according to Frances Wright, MD, Professor of Surgery at the University of Toronto and Sunnybrook Health Sciences Centre.
The two studies add to a growing body of evidence that properly conducted wellness programs are a win-win for patients and the health-care system, speakers said.
Postoperative Exercise Program
Dr. Wonders and colleagues examined the impact of a 12-week postsurgical program of individualized exercise aligned with the American College of Sports Medicine Guidelines for Cancer Survivors.1 They found program participants improved on all health-related quality-of-life measurements, whereas the control group declined or remained the same.
Although a number of studies have examined the relationship between exercise and well-being, this one is unique in evaluating how an exercise program may affect the use of health-care resources. Indeed, the study found that participation in the standardized program was significantly associated with a reduction in visits to the emergency department, hospital, and physician offices, resulting in lowered health-care costs.
The prospective clinical trial involved 243 patients randomly assigned to the supervised exercise program or to usual care in which patients received a resource guide. Interventions consisted of 150 minutes of cardiovascular exercise weekly, primarily walking, or recumbent bicycling at a low to moderate intensity. Each week, the group also engaged in two to three 60-minute sessions of full body workouts weekly using free weights or exercise stretch bands.
Groups were assessed before and after the intervention using the Functional Assessment of Cancer Therapy–Breast, the Short Form-36 Health Survey, and the Brief Fatigue Inventory. “These well-recognized measurement tools focus on physical, social, emotional, and functional well-being, rating performance on a scale of 1 to 28. Controlling for demographic factors and comorbidities, differences between the two groups were significant,” Dr. Wonders said.
KEY POINTS
- For breast cancer patients, participation in customized exercise and wellness programs around the time of surgery led to significant improvements in a variety of functional and quality-of-life measures.
- Patients in a supervised exercise program demonstrated significant reductions in emergency department visits, hospital visits, and doctor’s appointments, suggesting that such intervention affects the cost of health care for breast cancer.
Breast cancer–specific quality of life improved significantly across each category in the exercise group (P < .001). Most notably, there was a linear relationship between exercise and less use of health-care resources. Emergency department visits decreased by 33.2%; hospital outpatient visits, by 21.5%; and office-based visits, by 41.8%.
“With a growing recognition of the importance of exercise, currently it is written into the standards or guidelines of several major national U.S. breast cancer organizations,” she commented. “Our study adds to the body of literature supporting it, not only by demonstrating [patient] benefits but also by showing that exercise can help cut health-care costs.”
Prehabilitation During Neoadjuvant Chemotherapy
The study led by Dr. Wright evaluated the impact of individualized prehabilitation programs combining exercise with dietary and stress management counseling for patients with breast cancer undergoing neoadjuvant chemotherapy.2 The investigators studied the intervention’s efficacy on measures of functional aerobic capacity, quality of life, fatigue, disability, and pain.
“The goal of prehabilitation is to reduce the incidence and severity of current and future impairments,” Dr. Wright noted. Immediately after chemotherapy and 6 months after cancer surgery, program participants demonstrated improvements in functional walking capacity, self-reported general quality of life, measurements of fatigue, and other factors, compared with the control group.
In the study, 72 participants were randomly assigned to the intervention and control groups. The program was completed by 91% enrolled in active intervention and 84% in the usual-care group, with 86% of all women considered fully or partially adherent, among those who completed this data collection.
The intervention included the following components:
- Baseline assessment and individual counseling session with a nutritionist and periodic follow-up to optimize diet
- Baseline assessment with a psychiatrist to address anxiety and distress; a tool for guided daily meditation
- Customized exercise program that involved 3 to 5 days per week of moderate-level combined aerobic and resistance training in 30- to 40-minute sessions
- Education on smoking cessation and free nicotine replacement therapy if needed.
A variety of validated questionnaires were used to assess improvements in these areas. Table 1 shows some of the between-group differences in three key measures.
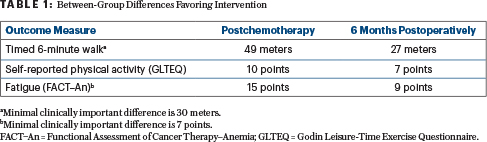
“The prehab group maintained their physical activity and, in fact, increased it 6 months later. Prehabilitation attenuated the worsening in fatigue by over two times,” she said. The program had few dropouts, no adverse events reported, and, according to qualitative interview data, a substantial positive impact on the treatment experience overall, she added.
“We still need an adequately powered trial to study the effectiveness of the intervention, especially using more sensitive measures of change for physical fitness,” Dr. Wright said. “However, our program will be operationalized shortly through a nonprofit that will offer it on a virtual platform nationally throughout Canada for women who wish to participate via a charity called Wellspring. We are very excited about the prospects.”
DISCLOSURE: Dr. Wonders and Dr. Wright reported no conflicts of interest.
REFERENCES
1. Wonders K, Schmitz K, Harness J, et al: The benefits of a clinically based individualized exercise oncology program on quality of life and health care costs for early-stage breast cancer patients. 2023 American Society of Breast Cancer Surgeons Annual Meeting. Abstract 1385675. Presented April 27, 2023.
2. Brahmbhatt P, Hong NL, Srikandarajah A, et al: A randomized control pilot of prehabilitation during neoadjuvant chemotherapy for women with breast cancer: A mixed methods study. 2023 American Society of Breast Cancer Surgeons Annual Meeting. Abstract 1387186. Presented April 27, 2023.

