Except in patients with no smoking history, the addition of chemotherapy to immunotherapy does not add benefit as a first-line treatment in patients with stage IV nonsquamous non–small cell lung cancer (NSCLC) and high expression of PD-L1, according to real-world experience.

Solange Peters, MD, PhD
Outcomes from the U.S. Flatiron Health database were presented at a European Society for Medical Oncology (ESMO) Virtual Plenary by Solange Peters, MD, PhD, Professor and Head of Medical Oncology at the Faculty of Biology and Medicine in Lausanne, Switzerland, and current President of ESMO.1
“Sparing chemotherapy in first-line chemoimmunotherapy did not appear to impact survival outcomes, except potentially in patients with no smoking history, where monotherapy performed significantly worse,” Dr. Peters reported. “For patients with PD-L1 ≥ 50%, I will use pembrolizumab or atezolizumab monotherapy.”
She added: “I find these data encouraging and reassuring, that monotherapy is a good option even in patients with brain or liver metastases, with the exception of never-smokers, who have to receive chemotherapy (and perhaps chemotherapy alone).”
Anti−PD-1/PD-L1 therapy alone and combined with platinum-based chemotherapy are front-line treatment options for patients with metastatic nonsquamous NSCLC with a PD-L1 tumor proportion score (TPS) ≥ 50%, ie, those with high PD-L1 expression. The determinants of what may be the optimal strategy in a given patient are unclear. To provide needed insight, Dr. Peters and colleagues examined outcomes from the real-world treatment of patients who had stage IV NSCLC with nonsquamous histology and PD-L1 TPS ≥ 50% treated with these approaches.
Flatiron Health Database of 520 Patients
Patients were identified from the Flatiron Health Electronic Health Record U.S. database; additional information was obtained from clinicians’ notes, biomarker reports, pathology reports, and the like. Researchers identified 24,075 patients with NSCLC, 520 of whom met the requirements of the study, most importantly stage IV disease (de novo or recurrence of stage I–III disease), nonsquamous histology, absence of a driver mutation, normal laboratory values, performance status of 0 to 2, PD-L1 ≥ 50%, and receipt in the first-line setting of immunotherapy alone or with platinum-based chemotherapy. Essentially all patients received pembrolizumab as the immunotherapy agent and carboplatin/pemetrexed as the chemotherapy regimen.
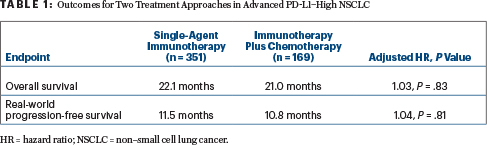
The population included 351 patients treated with a checkpoint inhibitor alone (essentially all pembrolizumab) and 169 treated with a checkpoint inhibitor plus platinum-based chemotherapy (essentially all carboplatin/pemetrexed). The primary endpoint was overall survival, and the key secondary endpoint was real-world progression-free survival. Hazard ratios (HRs) were adjusted for differences in baseline characteristics.
Propensity Score Weighting to Balance the Arms
The monotherapy arm contained a higher proportion of patients with poor prognostic baseline characteristics (notably, age and metastatic disease type [recurrent disease]) than the combination arm. Because of the small sample size and heterogeneity between treatment strategies within certain subgroups, the study excluded patients with squamous histology and those with PD-L1 of 1% to 49%.
The imbalance in patient characteristics between the two treatment groups was corrected through propensity score weighting, which took into account the following prognostic factors: age, sex, race, smoking history, performance status, type of metastasis, brain metastasis, liver metastasis, and time to treatment initiation.
“We have to accept that this is an observational study,” Dr. Peters acknowledged. “But, by using propensity weighting methodology, we have balanced patient characteristics as would have been done with randomization using stratification factors.”
Comparable Outcomes for Two Treatment Approaches
At a median follow-up of 23.5 months for the single-agent group and 19.9 months for the combination group, overall survival and real-world progression-free survival were not significantly different (Table 1).
“We saw absolutely superimposable overall survival curves for single-agent immunotherapy vs chemotherapy plus immunotherapy,” Dr. Peters reported. “But although the progression-free survival curves also look superimposable, we did see an excess of disease progression early after treatment was started, in favor of the chemotherapy-immunotherapy combination. This is a well-known phenomenon in monotherapy trials, and it did not reflect an impact on long-term overall survival or real-world progression-free survival benefit.”
In contrast to the overall results, there was a statistically significant and clinically meaningful improvement in overall survival and real-world progression-free survival in persons with no history of smoking, in whom combination therapy reduced these risks by 75% (P = .02 for treatment interaction) and 60% (P = .04 for treatment interaction), respectively.
In the other two subgroups of interest—patients with brain metastasis and liver metastasis—outcomes with the two treatments were similar. “The prognostic impact of brain metastasis might disappear in the era of immunotherapy. As for liver metastasis, apart from the well-known paradigm of liver metastasis representing a poor-prognosis group, we could not identify a difference in activity for monotherapy vs combination therapy, meaning that both are treatment options for these patients,” she said.
Median time to treatment discontinuation was 8.5 months in the monotherapy arm and 7.3 months in the combination arm. Any subsequent therapy was received by 31% and 33%, respectively.
DISCLOSURE: Dr. Peters has received institutional honoraria from AstraZeneca, Bristol Myers Squibb, Illumina, Medscape, MSD, Novartis, Pfizer, Roche, and Takeda; has served as an institutional consultant or advisor to AbbVie, Amgen, AstraZeneca, Bayer, Biocartis, Bioinvent, Blueprint Medicines, Boehringer Ingelheim, Bristol Myers Squibb, Clovis Oncology, Daiichi Sankyo, Debiopharm, Illumina, Incyte, Janssen, Lilly, Merck Serono, MSD, Novartis, Pfizer, Pharma Mar, Phosplatin Therapeutics, Regeneron, Roche/Genentech, Sanofi, Seattle Genetics, Takeda, and Vaccibody; has received institutional research funding from Amgen, AstraZeneca, Biodesix, Bristol Myers Squibb, Boehringer Ingelheim, Illumina, Iovance, Lilly, Merck Serono, MSD, Novartis, Pfizer, Phosplatin Therapeutics, and Roche; has been reimbursed for travel, accommodations, or other expenses by Bristol Myers Squibb, Incyte, MSD, Roche, and Sanofi; and has had uncompensated relationships with the Annals of Oncology, ESMO, the European Thoracic Oncology Platform, and the Journal of Thoracic Oncology.
REFERENCE
1. Peters S, Dafni U, Perol M, et al: Effectiveness of PD-(L)1 inhibitors alone or in combination with platinum-doublet chemotherapy in first-line non-squamous non-small cell lung cancer with PD-L1-high expression using real-world data. ESMO Virtual Plenary. Presented April 8, 2020.


