For over a decade, Patrick W. Mantyh, PhD, JD, has been investigating the molecular and cellular mechanisms that are involved in cancer-related pain, especially bone pain caused by advanced breast, prostate, and lung cancers. His early laboratory work using mouse models of bone cancer led to an understanding of the multiple mechanisms involved in the generation of pain, including allogeneic substances released from the cancer and its associated stromal cells as well as the destruction and sprouting of nerve fibers near the tumor.
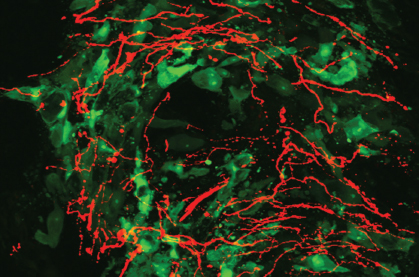
“Just as the tumor is constantly changing and evolving with disease, so too are the nerve fibers that innervate the tumor-bearing organ,” said Dr. Mantyh. “Tumors not only injure nerve fibers as they invade a tissue, they also cause a dramatic sprouting of sensory and sympathetic nerve fibers. Once you get this hyperinnervation of the cancer environment, if there are tumor and stromal factors being released that excite these nerve fibers, the cancer pain will continue to increase in intensity with time.”
These mechanistic insights into the causes of metastatic bone pain have led to the development of new treatments for bone pain, including bisphosphonates and denosumab (Prolia), antiresorptive compounds that simultaneously reduce bone cancer pain, tumor-induced bone destruction, and tumor growth within the bone; and anti–nerve growth factor (NGF) molecules, such as the monoclonal antibody tanezumab currently in phase III clinical trials.
The ASCO Post talked with Dr. Mantyh, Professor of Pharmacology at the University of Arizona Cancer Center in Tucson, about when pain management strategies should be started in the palliative care setting; what the most effective therapies are for controlling pain; and the emergence of targeted symptom therapy in alleviating cancer pain.
Start Pain Management Early
When should pain management strategies for patients in the palliative care setting be started, and how long should they last?
Pain management in the cancer setting should be started as early as possible and continue into survivorship. If chronic cancer pain is allowed to develop, not only will the pain fibers innervating the tumor-bearing organ change, both the spinal cord and higher centers of the brain will undergo reorganization, all of which contributes to further amplification of the pain.
In general, the earlier you effectively treat the pain, the less reorganization occurs, which makes the pain less severe and more tractable to effective control. The earlier you treat the pain, the easier it is for the clinician and the patient to control the pain, which can dramatically increase the quality of life and functional status of the patient.
‘Analgesic Ladder’
What is the most effective therapy for cancer pain management?
Currently, most cancer pain is managed using an “analgesic ladder,” which begins with nonsteroidal anti-inflammatory drugs (NSAIDs), then an NSAID plus a mild opiate, and, finally, when the pain becomes severe, an NSAID plus a strong opiate. In addition to this three-step ladder approach, adjuvant therapies, including steroids, radiation therapy, radioisotopes, nerve block, antiepileptics, and bisphosphonates, are commonly used in an attempt to control cancer pain.
Even with these therapies, cancer pain can be difficult to control fully 24/7, and the majority of patients with advanced cancer will still experience significant cancer pain. A major reason is because as the cancer advances, so too does the cancer pain, requiring ever-increasing doses of opiates.
Although opiates can be effective in controlling cancer pain, they also have many unwanted side effects, such as constipation, respiratory depression, and mental clouding, which can reduce a patient’s quality of life and functional status.
A Viable Therapeutic Target
Are pharmaceutical companies starting to develop specific targeted symptom therapies to control cancer pain?
With the development of preclinical models of cancer pain, enormous strides have been made in understanding the mechanisms that drive cancer pain. A little more than a decade ago, we had no idea of any specific mechanism that drove cancer pain. Now, we understand that acidosis, tumor-released products, and tumor-induced nerve reorganization all play major roles in driving cancer pain.
This increase in knowledge has allowed biotech and pharmaceutical companies to develop targeted therapies that have fewer side effects than opiates to treat cancer pain, such as bisphosphonates, denosumab, gabapentin, and anti-nerve growth factor therapies. And many other promising therapies are in development and in clinical trials. Thus, pharmaceutical and biotech companies now look upon cancer pain as a viable therapeutic target.
As patients with cancer are living much longer than ever before, targeted therapies to control cancer pain have the potential to dramatically improve their quality of life and functional status.
Pain Relief and Beyond
What is your current area of research?
We are focusing on developing more targeted therapies to relieve cancer pain. We are also attempting to understand whether unique mechanisms drive cancer pain in different types of cancer. For example, do the same mechanisms that drive bone cancer pain also drive head and neck cancer pain? Initial data suggest there are similarities in the mechanisms that drive pain in different cancer types, but just like the cancers themselves, there will probably be some unique aspects in pain arising from distinct cancers.
Another area we are exploring is whether novel therapies developed to relieve cancer pain also have significant effects on disease progression. Probably the best examples of these therapies are bisphosphonates and denosumab, which can reduce bone cancer pain and also significantly delay the time to cancer-induced bone fracture. Another example is radionuclide radium-223 chloride (Xofigo), which not only reduces bone pain from prostate cancer but also is associated with a clear increase in overall survival.
We are also very interested in the question of whether nerve fibers in bone are involved in metastasis of the tumor to bone as well as tumor vascularization and growth. For years, we have known that nerve fibers appear to serve as the scaffolding by which tumors escape from their primary site and metastasize to other organs. The two most studied examples of that are in prostate and pancreatic cancers. However, a study1 in Science investigating the role of nerves in prostate cancer growth and dissemination found that the formation of new nerve fibers within and around prostate tumors can alter tumor behavior and that nerves within the prostate promote early stages of tumorigenesis as well as cancer dissemination.
Do nerves in bone play a similar role in allowing metastatic tumors to preferentially metastasize, proliferate, and colonize the bone? We don’t know the answer to that yet, but given the importance of bone metastasis in many common cancers, this is an exciting time to be involved in the discovery and development of new therapies that decrease pain, improve quality of life, and potentially increase survival of patients with metastatic cancer. ■
Disclosure: Dr. Mantyh reported no potential conflicts of interest.
Reference
1. Magnon C, Hall SJ, Lin J, et al: Autonomic nerve development contributes to prostate cancer progression. Science 341:1236361, 2013.
Guest Editor
Addressing the evolving needs of cancer survivors at various stages of their illness and care, Palliative Care in Oncology is guest edited by Jamie H. Von Roenn, MD. Dr. Von Roenn is ASCO’s Senior Director of Education, Science and Professional Development Department.