The long-term benefits of radical prostatectomy vs watchful waiting in men with localized prostate cancer has remained a debated issue. As reported in The New England Journal of Medicine by Anna Bill-Axelson, MD, of Uppsala University Hospital, and colleagues, additional long-term follow-up in the Scandinavian Prostate Cancer Group-4 trial (SPCG-4) continues to show significant benefits of radical prostatectomy vs watchful waiting in early prostate cancer, including reduced risk of all-cause mortality, prostate cancer–specific mortality, and distant metastases and reduced need for androgen-deprivation therapy.1 Survival benefits have increased over time.
Study Details
In SPCG-4, 695 men with early prostate cancer were randomly assigned between 1989 and 1999 (ie, before the prostate-specific antigen [PSA] era) to radical prostatectomy or watchful waiting. The primary endpoints were death from any cause, death from prostate cancer, and risk of metastases; secondary endpoints included initiation of androgen-deprivation therapy. Patients in both groups had a mean age of 65 years, only 12% had nonpalpable T1c tumors at baseline, and mean PSA level was approximately 13 ng/mL.
Cumulative Mortality
By December 31, 2012, after a median follow-up of 13.4 years (range, 3 weeks to 23.2 years), a total of 294 men in the radical prostatectomy group had undergone radical prostatectomy (23 with node-positive disease did not undergo radical prostatectomy) and 294 men in the watchful waiting group had not received curative treatment. Totals of 200 men in the radical prostatectomy group and 247 in the watchful waiting group had died (18-year cumulative incidence = 56.1% vs 68.9%) and totals of 63 and 99 had died from prostate cancer (18-year cumulative incidence = 17.7% vs 28.7%).
Survival and Other Benefits
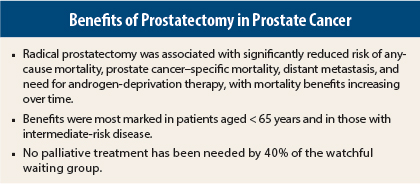
Patients in the radical prostatectomy group had significantly reduced risk of death from any cause (absolute 12.7% reduction, relative risk [RR] = 0.71, P < .001), death from prostate cancer (absolute 11.0% reduction, RR = 0.56, P = .001), and distant metastases (absolute 12.2% reduction, RR = 0.57, P < .001).
Patients in the radical prostatectomy group less frequently required androgen-deprivation therapy (absolute reduction 25.0%, RR = 0.49, P < .001). These patients also less frequently required other palliative treatments, including radiation therapy (14.1% vs 18.1%), chemotherapy (3.7% vs 4.9%), and laminectomy due to metastases (1.2% vs 2.6%).
Effect of Age and Tumor Risk
In subgroup analyses, reductions in any-cause mortality for prostatectomy were significant in patients under 65 years old (RR = 0.50, P < .001) and in patients with low-risk (RR = 0.57, P = .002) and intermediate-risk disease (HR = 0.71, P = .02). Reductions in risk for prostate cancer–specific mortality were significant in patients aged < 65 years (RR = 0.45, P = .002) and patients with intermediate-risk disease (RR = 0.38, P < .001).
Reduced risk of distant metastasis was significant both in patients aged < 65 years (RR = 0.49, P < .001) and in those aged ≥ 65 years (RR = 0.68, P = .04) as well as in patients with low-risk (RR = 0.40, P = .006) and intermediate-risk disease (HR = 0.49, P < .001). Patients in the prostatectomy group were significantly less likely to receive androgen-deprivation therapy in both age categories (RR = 0.39 for < 65 years and 0.60 for ≥ 65 years, both P < .001) and in all three risk categories (HR = 0.45 for each, P = .001 for low, P < .001 for intermediate and high).
Increased Benefits Over Time
Between 10 and 18 years of follow-up, the number needed to treat to prevent one death from any cause decreased from 20 to 8 in the whole cohort and from 8 to 4 in patients aged < 65 years. One patient died after surgery in the prostatectomy group. For prostate cancer–specific mortality, the difference favoring the prostatectomy group continued to increase from 9.6 deaths per 1,000 person-years during 5 to 10 years of follow-up to 24.5 deaths per 1,000 person-years during 15 to 20 years of follow-up.
The difference between groups in use of palliative treatment also increased with time. At 18 years, approximately 40% of men in the prostatectomy group and 60% in the watchful waiting group had disease progression with or without confirmed metastases and received androgen-deprivation therapy or other palliative treatments. The pattern for use of palliative treatments was similar in the < 65 and ≥ 65 year age groups.
The investigators concluded:
Extended follow-up 23 years after the initiation of the study corroborated a substantial reduction in the rate of death after radical prostatectomy. The number needed to treat to prevent one death has continued to decrease. The hypothesis-generating subgroup analyses and the large proportion of long-term survivors in the watchful waiting group who never required palliative treatment provide support for active surveillance as an alternative in adequately selected groups. However, the overall long-term disease burden is also a reminder that factors other than survival should be considered when counseling men with localized prostate cancer; the risk of metastases and ensuing palliative treatments also affect quality of life. ■
Disclosure: The study was supported by the Swedish Cancer Society, National Institutes of Health, Karolinska Institutet, Prostate Cancer Foundation, and Percy Falk Foundation. For full disclosures of the study authors, visit www.nejm.org.
Reference
1. Bill-Axelson A, Holmberg L, Garmo H, et al: Radical prostatectomy or watchful waiting in early prostate cancer. N Engl J Med 370:932-942, 2014.