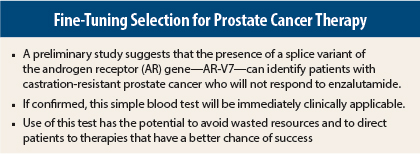
A simple blood test may be able to identify men with castration-resistant prostate cancer who will not respond to enzalutamide (Xtandi). The presence of the splice variant androgen receptor (AR) V7 in circulating tumor cells identified men who were unlikely to respond to enzalutamide and whose disease would progress more quickly, according to an early study presented at the 2014 Annual Meeting of the American Association for Cancer Research (AACR) in San Diego.1 This was the first presentation of these data.
“AR-V7 is detectable in [circulating tumor cells] in a subset of [castration-resistant prostate cancer] patients and seems to predict resistance to enzalutamide. We believe these data have immediate clinical implications in that we can steer patients who test positive for this splice variant away from enzalutamide and offer them chemotherapy and/or radiation,” said Emmanuel S. Antonarakis, MD, Assistant Professor of Oncology at Johns Hopkins Sidney Kimmel Comprehensive Cancer Center, Baltimore.
“Further, the availability of a blood biomarker for AR-V7 could fuel the development of novel therapies targeting this aberrant version of the androgen receptor.”
Multiple Mechanisms
During the discussion following this presentation, Dr. Antonarakis said that there are multiple potential mechanisms responsible for resistance. “We are not postulating that AR-V7 is the only mechanism of resistance to enzalutamide in [castration-resistant prostate cancer] patients,” he noted.
“[Castration-resistant prostate cancer] may be a misnomer, because a number of men with this disease continue to benefit from a variety of [androgen receptor]-directed therapies. This implies that [castration-resistant prostate cancer] remains androgen-driven. Enzalutamide inhibits the binding of androgens to the androgen receptor and inhibits nuclear translocation of the androgen receptor. It has been hailed as a miracle drug for some patients, but a significant proportion of patients do not benefit from this agent,” he said.
Use of enzalutamide for castration-resistant prostate cancer in the predocetaxel setting is off-label. However, U.S. Food and Drug Administration (FDA) approval for this indication may soon be forthcoming.
In the phase III AFFIRM study that led to initial FDA approval of enzalutamide, 21% of patients failed to respond, based on no appreciable decline in prostate-specific antigen (PSA) levels. Although many potential reasons for resistance to the drug have been proposed, Dr. Antonarakis and his colleagues have focused on splice variants of the androgen receptor as one mechanism of resistance. To date, 18 different androgen receptor splice variants have been described.
“We believe AR-V7 is the most important variant. These variants are missing the ligand binding domain, which is the direct target of enzalutamide,” he continued.
Key Data
The study employed a circulating tumor cell–based AR-V7 assay that has two parts: the Adna Test Prostate Cancer Select and the Adna Test Prostate Cancer Detect kits (Adna Gen, Langenhagen, Germany). A total of 31 men with castration-resistant prostate cancer about to start treatment with enzalutamide were prospectively enrolled. They provided circulating tumor cell samples at baseline, at the time of response, and at the time of resistance. At the AACR meeting, Dr. Antonarakis presented data only on the baseline samples.
Of the 31 patients, 12 (39%) had detectable AR-V7 in their circulating tumor cells; 61% did not. Among patients previously treated with abiraterone (Zytiga), the incidence of detectable AR-V7 increased to 55%, whereas it was detectable in only 9% of those who were abiraterone-naive.
None of the patients with detectable AR-V7 responded to enzalutamide according to RECIST criteria or PSA criteria. Every patient who had a prostate-specific antigen (PSA) response had wild-type AR, although presence of wild-type AR only did not guarantee a response. In addition, the presence of detectable AR-V7 was associated with a 7.4-fold risk of PSA progression and an 8.5-fold risk of clinical/radiographic progression, compared to patients with wild-type AR only.
In a multivariate model for response, three factors were independently associated with inferior response: detectable AR-V7, baseline PSA level, and previous abiraterone treatment. In another multivariate assessment, two factors were associated with progression-free survival: the presence of AR-V7 and previous abiraterone therapy. ■
Disclosure: Dr. Antonarakis reported no potential conflicts of interest.
Reference
1. Antonarakis E, Lu C, Wang H, et al: 2014 AACR Annual Meeting. Abstract 2910. Presented April 7, 2014.