Detection of depression is suboptimal, and its severity is underestimated in the general population, but it is known psychiatric disorders are more common in patients with cancer than in those with any other chronic illness. Although studies in cancer patients have yielded varying figures, it is estimated that point prevalences among cancer patients are 20.7% for any mood disorder, 10.3% for anxiety disorder, and 19.4% for any adjustment disorder.
ASCO has adapted the Pan-Canadian Practice Guideline on Screening, Assessment, and Care of Psychosocial Distress (Depression, Anxiety) in Adults With Cancer1 for use in the screening, assessment, and care of anxiety and depressive symptoms in adults with cancer.2 The adapted guideline, reported in the Journal of Clinical Oncology, applies to patients aged ≥ 18 years at any phase of the cancer continuum and regardless of cancer type, disease stage, or treatment modality, and it is targeted to professional health-care providers including medical, surgical, and radiation oncologists, psychiatrists, psychologists, primary care providers, nurses, and others involved in care, as well as to patients, family members, and caregivers.
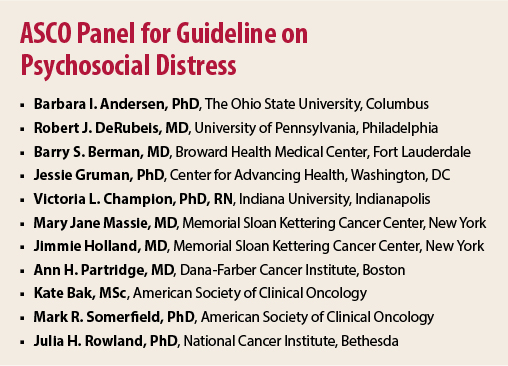
The pan-Canadian guideline underwent methodologic review by ASCO senior guideline staff members and content review by an ASCO ad hoc panel including multidisciplinary representation. The expert panel was co-chaired by Barbara L. Andersen, PhD, The Ohio State University, Columbus, and Julia Howe Rowland, PhD, of the National Cancer Institute.
Guideline Principles
The final recommendations of the adapted guideline are as follows:
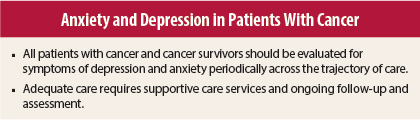
- All patients with cancer and cancer survivors should be evaluated for symptoms of depression and anxiety periodically across the trajectory of care. Assessment should be performed using validated measures. Depending on levels of symptoms, different treatment pathways are recommended (see below). Failure to identify and treat anxiety and depression in cancer patients increases the risk of poor quality of life and, potentially, risk of disease-related morbidity and mortality.
- Health-care practitioners implementing the guideline recommendations should first identify the available resources in their institution and community for the treatment of depressive and anxiety symptoms. The availability and accessibility of supportive care services are important in preventing or reducing the severity of symptoms of psychopathology.
It is recommended that patients be screened for depression and anxiety at diagnosis, at regular intervals thereafter, and as needed. Assessments should be a shared responsibility of a clinical team. Concerns such as risk of harm to self and/or others, severe depression or agitation, or the presence of psychosis or confusion warrant immediate referral to a psychiatrist, psychologist, physician, or equivalently trained professional.
The recommended assessment instruments are the nine-item Personal Health Questionnaire (PHQ)-9 for depression and the seven-item Generalized Anxiety Disorder (GAD)-7 scale for anxiety. The adapted guideline lists other assessment instruments that can be used.
Depression
Initial assessment should be performed with two items from the PHQ-9 regarding whether the patient has felt little interest or pleasure in activities (anhedonia) and has felt down, depressed, or helpless (depressed mood). Patients with scores indicating presence of anhedonia or depressed mood should complete the remainder of the PHQ-9. Other patients require no further screening.
Scores on the PHQ-9 categorize patients as having no/mild symptoms (1–7), moderate symptoms (8–14), or moderate-to-severe (15–19) or severe (20–27) symptoms. Patients with moderate or greater symptomatology should have further diagnostic assessment to identify the nature and extent of the depressive symptoms and the presence or absence of a mood disorder.
Patients with no/mild symptoms should enter Care Pathway 1—supportive care and prevention—and be offered referral to supportive care services (see below).
Patients with moderate symptoms should enter Care Pathway 2—psychological (group) or psychosocial intervention. Low-intensity intervention options for these patients include individually guided self-help based on cognitive-behavioral therapy (including behavioral activation and problem-solving), group-based cognitive-behavioral therapy for depression, group psychosocial intervention, and pharmacologic treatment (as appropriate).
Patients with moderate-to-severe or severe symptomatology should enter Care Pathway 3, consisting of individual psychological or psychiatric intervention. The high-intensity interventions in this setting include individual cognitive-behavioral therapy or interpersonal therapy, pharmacologic treatment, or both. All patients with moderate or worse symptoms should be referred to supportive care services.
Anxiety
Patients should initially be assessed with the GAD-7 scale. Scores on GAD-7 categorize patients as having no/mild symptoms (0–9), moderate symptoms (10–14), or moderate-to-severe or severe symptoms (15–21). Those with no/mild symptoms should be offered referral to supportive care. Low-intensity interventions in those with moderate symptoms include education and active monitoring, nonfacilitated or guided self-help based on cognitive-behavioral therapy, group psychosocial intervention, and pharmacologic intervention (as appropriate).
High-intensity interventions in those with moderate-to-severe or severe symptoms include individual psychologic treatment with cognitive-behavioral therapy or applied relaxation, pharmacologic treatment, or both. All patients with moderate or worse symptoms should be referred to supportive care services.
Supportive Care Services
Education and information should be provided for the patient and family regarding:
- Normalcy of stress in the context of cancer
- Specific stress-reduction strategies (eg, progressive muscle relaxation)
- Sources of informational support/resources (patient library, reliable Internet sites)
- Availability of supportive care services (eg, professionally led groups, informational lectures, volunteer organizations) at the institution or in the community
- Availability of financial support (eg, accommodations, transportation, health/drug benefits)
- Information about signs and symptoms of depression if stress or distress worsen and avenues for depression care, or information about signs and symptoms of anxiety disorders and their treatment
- Information on sleep hygiene and self-management of fatigue
- Information on other nonpharmacologic interventions (physical activity, nutrition)
Follow-up and Ongoing Assessment
As noted in the adapted guideline, it is common for persons with depressive symptoms to lack the motivation needed to follow through on referrals or to comply with treatment recommendations. Similar considerations apply to persons with anxiety, since cautiousness and tendency to avoid threatening stimuli are primary features of the pathology. Thus, it is recommended that the following measures be taken on a biweekly or monthly basis or until symptoms have remitted in patients with depressive symptoms and on a monthly basis or until symptoms have subsided in those with anxiety:
- Assessment of follow-through and compliance with individual or group psychological/psychosocial referrals, as well as satisfaction with these services
- Assessment of compliance with pharmacologic treatment, patient’s concerns about side effects, and satisfaction with the symptom relief
- If compliance is poor, assessment and construction of a plan to circumvent obstacles to compliance, or discussion of alternative interventions that present fewer obstacles
- Change in the treatment course (eg, addition of psychological or pharmacologic intervention, change of specific medication, referral to individual psychotherapy if group therapy has not proved helpful) if symptom reduction and satisfaction with treatment are poor, despite good compliance, after 8 weeks of treatment
- For patients with anxiety, consideration of tapering from antidepressant medications if anxiety symptoms are under control and if the primary environmental sources of anxiety are no longer present
The panel stated, “Although clinicians may not be able to prevent some of the chronic or late medical effects of cancer, they have a vital role in mitigating the negative emotional and behavioral sequelae. Recognizing and treating effectively those who manifest symptoms of anxiety or depression will reduce the human cost of cancer.” ■
Disclosure: The authors reported no potential conflicts of interest.
References
1. Howell D, Keller-Olaman S, Oliver T, et al: A pan-Canadian practice guideline: Screening, assessment and care of psychosocial distress (depression, anxiety) in adults with cancer. Canadian Partnership Against Cancer (Cancer Journey Action Group) and the Canadian Association of Psychosocial Oncology, 2010. Available at www.capo.ca.
2. Andersen BL, DeRubeis RJ, Berman BS, et al: Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: An American Society of Clinical Oncology Guideline Adaptation. J Clin Oncol. April 14, 2014 (early release online).