 Cisplatin-based adjuvant therapy is recommended for patients with resected stage II–IIIA non–small cell lung cancer (NSCLC). There have been no trials of adjuvant therapy in elderly patients with NSCLC, who constitute a large part of the NSCLC population. A number of analyses indicate that older patients benefit from adjuvant therapy with acceptable toxicity, including a retrospective analysis of the National Cancer Institute of Canada and Intergroup Study JBR.10 trial1 and the Lung Adjuvant Cisplatin Evaluation (LACE) meta-analysis.2 However, it remains unclear to what degree such patients are receiving adjuvant therapy in clinical practice.
Cisplatin-based adjuvant therapy is recommended for patients with resected stage II–IIIA non–small cell lung cancer (NSCLC). There have been no trials of adjuvant therapy in elderly patients with NSCLC, who constitute a large part of the NSCLC population. A number of analyses indicate that older patients benefit from adjuvant therapy with acceptable toxicity, including a retrospective analysis of the National Cancer Institute of Canada and Intergroup Study JBR.10 trial1 and the Lung Adjuvant Cisplatin Evaluation (LACE) meta-analysis.2 However, it remains unclear to what degree such patients are receiving adjuvant therapy in clinical practice.
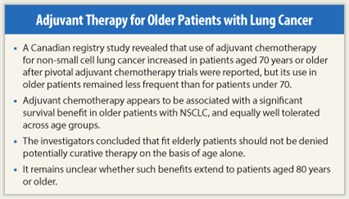
In a population-based, retrospective cohort study recently reported in the Journal of Clinical Oncology, Cuffe and colleagues3 analyzed uptake of adjuvant therapy and outcomes by age in patients with NSCLC undergoing surgical resection during the periods 2001–2003 and 2004–2006. The study found that use of adjuvant therapy in elderly patients (age ≥ 70 years) increased across the two periods and appeared to be associated with a survival advantage. Nevertheless, the study also found that use of adjuvant therapy in the elderly still lags behind that in younger patients.
Patient Characteristics
Using the Ontario Cancer Registry, the investigators identified 6,570 NSCLC cases treated with surgical resection from 2001 to 2006.3 Between the periods 2001–2003 and 2004–2006, the proportion of surgical cases who were elderly (age ≥ 70 years) increased from 42.5% to 45.0% (P = .006). After exclusion of patients who received preoperative therapy, 2,763 (43.8%) of 6,304 surgical cases were aged 70 years or older, with 1,317 aged 70 to 74 years, 980 aged 75 to 79 years, and 466 aged 80 years or older.
Elderly patients were significantly more likely to be male and to have comorbidities, longer postoperative inpatient stays, and squamous histology. They were significantly less likely to be treated at regional cancer centers, to undergo pneumonectomy or postoperative radiotherapy, and to have adenocarcinoma. For the periods 2001–2003 and 2004–2006, respectively, 1,697 and 1,844 patients were aged less than 70 years, 623 and 694 were aged 70 to 74 years, 446 and 534 were aged 75 to 79 years, and 184 and 282 were aged 80 years or older.
Key Findings
Use of adjuvant chemotherapy in the elderly population increased from 3.3% to 16.2% between 2001–2003 (hence, the pre–adjuvant therapy adoption cohort) and 2004–2006 (postadoption cohort). However, the proportions of patients receving adjuvant therapy during 2004–2006 still showed a significant decrease with increasing age, from 42.7% in those aged less than 70 years, to 23.1% in those aged 70 to 74 years, 13.3% in those aged 75 to 79 years, and 4.6% in those aged 80 years or more (P < .001). For elderly patients in the postadoption cohort, factors associated with increased likelihood of adjuvant therapy use included shorter postoperative inpatient stay and (consistent with guideline recommendations) stage II/III disease. Adjuvant therapy use varied significantly by region of Ontario, ranging from 9.3% to 28.4%.
On multivariate analysis, factors significantly associated with likelihood of receiving adjuvant therapy among elderly patients were geographic location, pathologic stage, and advancing age (all P < .001). The investigators found no significant association between Charlson comorbidity score and use of adjuvant therapy in the elderly, although they did see a trend toward decreased use of adjuvant therapy in patients with three or more comorbidities.
Detailed data on chemotherapy were available from 584 patients treated at regional centers in 2004–2006. Cisplatin/vinorelbine was the most commonly used regimen across all age groups. However, carboplatin-based regimens were used significantly more frequently in elderly patients, accounting for treatment in 7% of patients aged less than 70 years, compared with 18% of those aged 70 to 74 and 75 to 79 years and 29% of those aged 80 years or older (P = .007). Chemotherapy appeared to be equally well tolerated across age groups, with no significant age-related differences being observed in frequency of changing from cisplatin to carboplatin or other drugs, or in frequency of dose reduction or interruption.
Survival and Toxicity
Four-year overall survival improved from 52.5% in the preadoption cohort (patients undergoing resection in 2001–2003) to 56.1% in the postadoption cohort (those undergoing resection in 2004–2006; P = .001). Overall survival in elderly patients improved from 47.1% in the preadoption cohort to 49.9% in the postadoption cohort (P = .01). Compared with the preadoption cohort, risk for death in the postadoption cohort was significantly reduced by 15% (HR = 0.85, P = .0029) in patients aged less than 70 years and by 13% (HR = 0.87, P = .0122) in all patients aged 70 years or older. In the elderly patient age groups, risk for death was significantly reduced by 17% (HR = 0.83, P = .0271) in those aged 70 to 74 years and by a borderline significant 16% (HR = 0.84, P = .0517) in those aged 75 to 79 years, whereas there was no reduction in risk in patients aged 80 years or older (HR = 1.00, P = NS).
Treatment-related toxicity was assessed by evaluating hospital admissions within 6 months after surgery. Compared with the preadoption cohort, hospitalizations within 6 months after surgery declined in elderly patients in the postadoption cohort (40.0% vs 38.3%), suggesting that more common use of adjuvant therapy did not increase treatment-related toxicity.
 In the postadoption cohort, elderly patients were more likely than younger patients to be hospitalized within 6 weeks after surgery, with hospitalization occurring in 11.1% of patients aged less than 70 years, compared with 12.1% of those aged 70 to 74 years, 17.2% of those aged 75 to 79 years, and 17.7% of those aged 80 years or older (P = .0002). This finding suggests that surgical morbidity was greater in elderly patients, at least those aged 75 years or older. However, during the period from 6 weeks to 6 months after surgery—ie, the period during which patients were most likely to be receiving adjuvant therapy—there was no difference in rates of hospitalization between nonelderly and elderly patients. During this period, 28.0% of patients aged less than 70 years were admitted to the hospital, compared with 26.6% of those aged 70 to 74 years, 27.6% of those aged 75 to 79 years, and 31.5% of those aged 80 years or older.
In the postadoption cohort, elderly patients were more likely than younger patients to be hospitalized within 6 weeks after surgery, with hospitalization occurring in 11.1% of patients aged less than 70 years, compared with 12.1% of those aged 70 to 74 years, 17.2% of those aged 75 to 79 years, and 17.7% of those aged 80 years or older (P = .0002). This finding suggests that surgical morbidity was greater in elderly patients, at least those aged 75 years or older. However, during the period from 6 weeks to 6 months after surgery—ie, the period during which patients were most likely to be receiving adjuvant therapy—there was no difference in rates of hospitalization between nonelderly and elderly patients. During this period, 28.0% of patients aged less than 70 years were admitted to the hospital, compared with 26.6% of those aged 70 to 74 years, 27.6% of those aged 75 to 79 years, and 31.5% of those aged 80 years or older.
Study Implications
As stated by the authors, these findings suggest that the benefits of adjuvant therapy in elderly patients that have been identified in analyses of clinical trials are being realized in general practice—although it remains unclear whether such benefits extend to patients aged 80 years or older. However, the findings also indicate that adoption of adjuvant therapy lags in the elderly. The investigators noted, “Significant efforts … are necessary to improve understanding of the reasons underlying this apparent low utilization in the elderly and to promote referral of such patients to medical oncology to ensure that fit elderly patients are not denied potentially curative therapy on the basis of age alone.” ■
References
1. Pepe C, Hasan B, Winton TL, et al: Adjuvant vinorelbine and cisplatin in elderly patients: National Cancer Institute of Canada and Intergroup Study JBR.10. J Clin Oncol 25:1553-1561, 2007.
2. Fruh M, Rolland E, Pignon JP, et al: Pooled analysis of the effect of age on adjuvant cisplatin-based chemotherapy for completely resected non-small-cell lung cancer. J Clin Oncol 26:3573-3581, 2008.
3. Cuffe S, Booth CM, Peng Y, et al: Adjuvant chemotherapy for non-small cell lung cancer in the elderly: A population-based study in Ontario, Canada. J Clin Oncol. April 23, 2012 (early release online).

