GUEST EDITORS

Syed A. Abutalib, MD

L. Jeffrey Medeiros, MD
Dr. Abutalib is Assistant Director, Hematology and Hematopoietic Cell Transplantation Director, Hematopoietic Cell Transplant Apheresis Service, Cancer Treatment Centers of America, Zion, Illinois, Editor-in-Chief, Advances in Cell & Gene Therapy. Dr. Medeiros is Professor and Chair, Department of Hematopathology, The University of Texas MD Anderson Cancer
Center, Houston.
The ASCO Post is pleased to present Hematology Expert Review, an ongoing feature that quizzes readers on issues in hematology. In this installment, Drs. Abutalib and Medeiros explore the updated World Health Organization (WHO) classification of hematopoietic and lymphoid tissue malignancies, focusing on primary myelofibrosis. For each quiz question that follows, select the one best answer. The correct answers and accompanying discussions appear below.
Question 1
Which of the following is an important finding in establishing the diagnosis of prefibrotic/early-stage primary myelofibrosis?
A. Increased proliferation of megakaryocytes in the bone marrow
B. Absence of MPL mutation
C. Decreased age-adjusted bone marrow cellularity
D. Absence of either ASXL1 or SRSF2 mutation
Question 2
Which of the following morphologic feature(s) distinguishes essential thrombocythemia from prefibrotic/early-stage primary myelofibrosis?
A. The myeloid-to-erythroid ratio is normal in essential thrombocythemia and increased in prefibrotic/early primary myelofibrosis.
B. Age-adjusted bone marrow cellularity is normal in essential thrombocythemia and increased in prefibrotic/early primary myelofibrosis.
C. Megakaryocytes are large and have hyperlobulated nuclei in essential thrombocythemia and are variably sized and have hypolobulated nuclei in prefibrotic/early primary myelofibrosis.
D. All of the above.
Question 3
Approximately what proportion of patients with primary myelofibrosis harbor CALR mutation?
A. 0%
B. 1% to 5%
C. 20% to 30%
D. 60% to 70%
Question 4
A person with primary myelofibrosis can present without which of the following clinical or laboratory finding(s)?
A. Anemia
B. Leukocytosis
C. Hepatomegaly
D. All of the above
Answers to Hematology Expert Review Questions
Question 1
Which of the following is an important finding in establishing the diagnosis of prefibrotic/early-stage primary myelofibrosis?
Correct answer: A. Increased proliferation of megakaryocytes in the bone marrow.
Expert Perspective
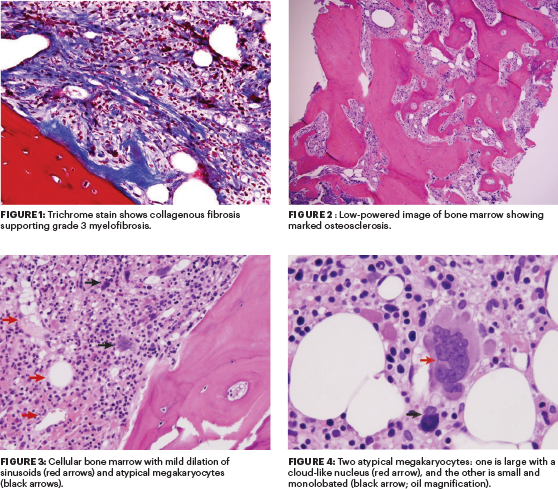
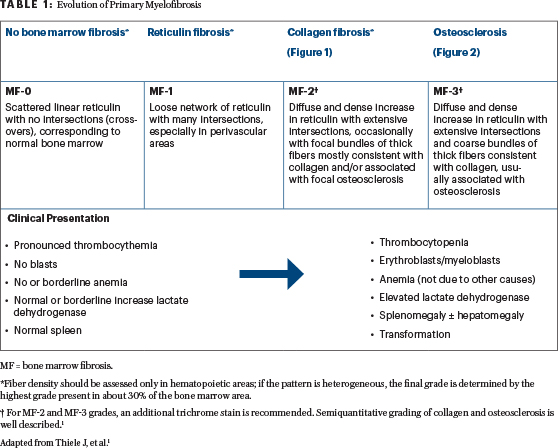
Approximately 30% to 50% of primary myelofibrosis cases are first detected in the prefibrotic/early stage, with no significant increase in reticulin and/or collagen fibers (ie, fibrosis grades 0 and 1 [Table 1, Figures 1 and 2]).1-3 Hence, it is important for treating health-care providers to familiarize themselves with the WHO diagnostic criteria.
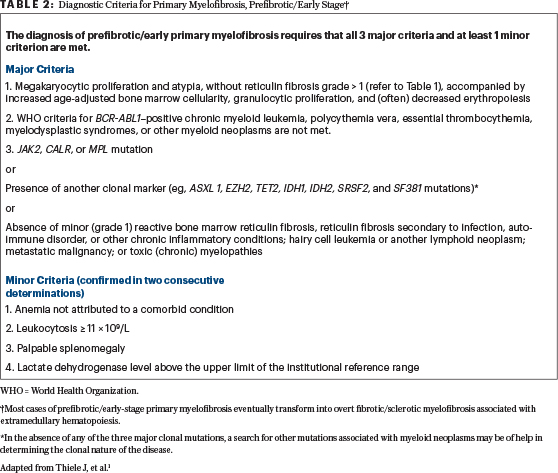
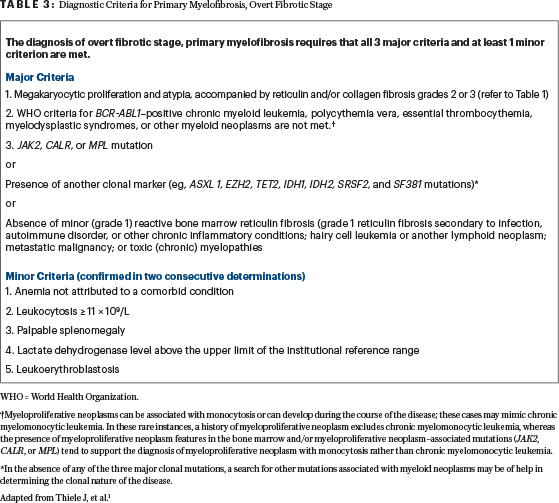
In the bone marrow examination, the megakaryocytes are markedly abnormal, and their morphologic atypia and topographic distribution within the bone marrow are critical for the recognition of prefibrotic (early stage) primary myelofibrosis. The megakaryocytes often form dense clusters, which are frequently adjacent to the bone marrow vascular sinuses and bone trabeculae (Figure 3).1 Most megakaryocytes are enlarged, but small megakaryocytes may also be seen, as they vary in size. Deviations from the normal nuclear-to-cytoplasmic ratio (an indication of defective maturation), abnormal patterns of chromatin clumping (including hyperchromatic forms and bulbous, cloud-like, or balloon-shaped nuclei), and the frequent occurrence of bare (naked) megakaryocyte nuclei are typical findings. Overall, in prefibrotic primary myelofibrosis, the megakaryocytes are more atypical than in any other type of myeloproliferative neoplasm (Figure 4).
All of these morphologic findings are accompanied by increased age-adjusted bone marrow cellularity, granulocytic proliferation, and (often) decreased erythropoiesis. The presence of a clonal marker (eg, JAK2, CALR, or MPL) is one of the three major criteria for diagnosis of primary myelofibrosis (Tables 2 and 3).1
Question 2
Which of the following morphological feature(s) distinguishes essential thrombocythemia from prefibrotic/early-stage primary myelofibrosis.
Correct answer: D. All of the above.
Expert Perspective
No single morphologic feature is pathognomonic for either essential thrombocythemia or prefibrotic/early-stage primary myelofibrosis, but the identification of characteristic morphologic patterns is the key to distinguishing between the two disease entities.1 Thus, choices A, B, and C are correct.
Question 3
Approximately what proportion of patients with primary myelofibrosis harbor CALR mutation?
Correct Answer: C. 20% to 30%.
Expert Perspective
In WHO-defined primary myelofibrosis, JAK2 V617F mutation is found in 50% to 60% of early-stage cases (as well as in advanced stages)1; CALR mutations are found in about 24% of primary myelofibrosis cases, and MPL mutations are found in 8%. About 12% of cases are triple-negative for mutations in JAK2,CALR, and MPL.1,4 Although these mutations are helpful in distinguishing primary myelofibrosis from reactive conditions that can result in bone marrow fibrosis, they are not specific for primary myelofibrosis; mutations in these genes can also be found in essential thrombocythemia, and JAK2 V617F can be found in polycythemia vera.1,4
Question 4
A person with primary myelofibrosis can present without which of the following clinical or laboratory finding(s)?
Correct answer: D. All of the above.
Expert Perspective
In the initial prefibrotic stage/early stage of primary myelofibrosis, the only finding may be marked thrombocytosis mimicking essential thrombocythemia, because the other clinical features may be either within the normal range or borderline abnormal (Table 1).1 Neither sustained thrombocytosis nor positive mutation status alone can distinguish prefibrotic primary myelofibrosis from essential thrombocythemia, but careful analysis of bone marrow morphology can be, and therefore is, a necessary procedure.
It is prudent to recognize that approximately 30% of primary myelofibrosis cases are asymptomatic at the time of diagnosis and are discovered by detection of splenomegaly during a routine physical examination or when a routine blood cell count reveals anemia, leukocytosis, and/or thrombocytosis. Splenomegaly of various degrees is detected in as many as 90% of patients, and it can be massive.1 Approximately 50% of patients have hepatomegaly, depending on the stage (prefibrotic/early or fibrotic/advanced) of the disease.1 ■
DISCLOSURE: Dr. Abutalib is an advisor for AstraZeneca. Dr. Medeiros reported no conflicts of interest.
REFERENCES
1. Thiele J, Kvasnicka HM, Orazi A, et al: Polycythemia vera, in Swerdlow SH, Campo E, Harris NL, et al (eds.): WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, pp 39-53. Lyon, France, International Agency for Research in Cancer, 2017.
2. Barosi G: Essential thrombocythemia vs. early/prefibrotic myelofibrosis: Why does it matter. Best Pract Res Clin Haematol 27:129-140, 2014.
3. Thiele J, Kvasnicka HM: Prefibrotic chronic idiopathic myelofibrosis: A diagnostic enigma? Acta Haematol 111:155-159, 2004.
4. Tefferi A, Guglielmelli P, Larson DR, et al: Long-term survival and blast transformation in molecularly annotated essential thrombocythemia, polycythemia vera, and myelofibrosis. Blood 124:2507-2513, 2014.

