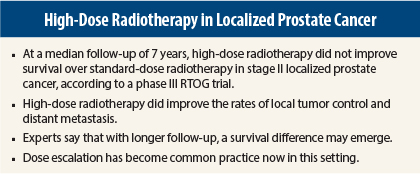
High-dose radiotherapy failed to improve overall survival at 7 years compared with standard-dose radiotherapy in men with stage II localized prostate cancer. However, the high-dose schedule had several advantages, including improved rates of local tumor control and distant metastasis, according to the results of the phase III Radiation Therapy Oncology Group (RTOG) 0126 study1 presented at the 2015 Genitourinary Cancers Symposium.
“We were disappointed that we failed to see an improvement in overall survival,” said lead author Jeff M. Michalski, MD, of Washington University School of Medicine, St. Louis. “Dose escalation did not significantly decrease the rate of death from prostate cancer. However, dose escalation does offer some valuable outcomes, just not improvement in survival,” he added.
Study Details
At a median follow-up of 7 years, the 5-year overall survival rates were 88% and 89% in the high-dose and standard radiotherapy arms, respectively, and 10-year overall survival rates were 67% and 66% in the high-dose and standard arms, respectively. These differences were not statistically significant.
RTOG 0126 evaluated whether a 79.2-Gy dose of three-dimensional conformal radiotherapy (3D-CRT) or intensity-modulated radiotherapy improved overall survival compared with the standard 3D-CRT or intensity-modulated radiotherapy dose of 70.2 Gy. The 79.2-Gy dose was chosen for the trial because it had been previously identified as feasible and associated with fewer side effects than other dose schedules, Dr. Michalski said.
A total of 1,532 patients were randomized 1:1 to receive either 44 fractions of high-dose radiotherapy or 39 fractions of standard radiotherapy. The median age of patients was 69 years, and 66% received 3D-CRT. No patient received hormone therapy.
Meaningful Improvements
High-dose radiotherapy did show improvements over standard therapy regarding the rates of biochemical failure, distant metastasis, and time to local tumor progression. Ten-year rates of biochemical failure were 30% and 45% in the high-dose and standard radiotherapy arms, respectively (P < .0001).
Ten-year rates of time to local tumor progression were 4% and 8% in the high-dose and standard radiotherapy arms, respectively (P = .0059), and the 10-year rates of distant metastasis were 5% and 8% in the high-dose and standard arms, respectively (P = .026).
Less salvage therapy was used in the high-dose radiotherapy arm (13.5% vs 20.6%, P = .0002).
High-dose radiotherapy incurred greater late toxicity, including grade 2 or higher gastrointestinal and genitourinary adverse events. Dr. Michalski said there are strategies that can reduce these side effects such as intensity-modulated radiotherapy and careful attention to rectal dosimetry.
Further study is planned to test dose-escalated therapy. The RTOG 0815 trial, completing accrual, will evaluate dose-escalated radiotherapy with or without a short course of androgen-deprivation therapy. ■
Disclosure: Dr. Michalski reported no potential conflicts of interest.
Reference
1. Michalski JM, Moughan J, Purdy J, et al: A randomized trial of 79.2 Gy versus 70.2 Gy radiation therapy for localized prostate cancer. 2015 Genitourinary Cancers Symposium. Abstract 4. Presented February 26, 2015.