The monoclonal antibody gemtuzumab ozogamicin (Mylotarg) improved event-free survival and reduced the risk of relapse in children with acute myeloid leukemia (AML) in a study from the Children’s Oncology Group, presented at the 55th American Society of Hematology (ASH) Annual Meeting and Exposition by Alan S. Gamis, MD, MPH, Associate Director of Hematology/Oncology and Section Chief of Oncology at Children’s Mercy Hospitals and Clinics in Kansas City, Missouri.1
“Gemtuzumab ozogamicin improved event-free survival in children, adolescents, and young adults with AML by reducing the risk of relapse among those achieving remission,” Dr. Gamis reported.
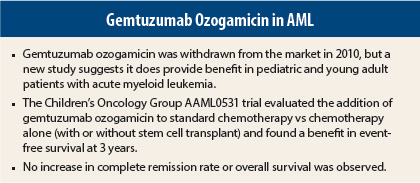
Initial findings for gemtuzumab ozogamicin, the first humanized anti-CD33 monoclonal antibody, were so promising in treatment-refractory patients that the drug was granted accelerated approval in 2000. Subsequent phase III clinical trials, however, failed to replicate the positive results in newly diagnosed patients, leading to the drug’s withdrawal from the market in 2010. Two subsequent trials were again contradictory, showing that disease-free survival and reduced risk of relapse did, indeed, occur with gemtuzumab ozogamicin, primarily in the low- or intermediate-risk AML subgroups, according to Dr. Gamis.
“We know that AML is a very heterogeneous disease, and thus, we don’t expect one single agent to work in all patients,” Dr. Gamis said, “so this endpoint was designed to look at whether gemtuzumab ozogamicin improves event-free survival from the time of diagnosis, and whether this benefit varied by risk group method of intensification.”
Study Details
The phase III AAML0531 trial enrolled 1,070 pediatric and young adult patients (median age, 10 years), randomly assigning them to standard therapy alone or to two doses of gemtuzumab ozogamicin at 3 mg/m2 per dose on day 6 of induction and on day 7 of intensification, with a five-cycle chemotherapy backbone. The use of stem cell transplantation was stratified by risk, with high-risk patients allocated to best allogeneic donor transplant after the first induction, while low-risk patients received chemotherapy only and intermediate-risk patients were assigned to transplant if there was a matched family donor.
After a median follow-up of 3.5 years, the 3-year event-free survival rate from time of study entry was 53.1% in the gemtuzumab ozogamicin arm vs 46.9% in the standard treatment arm, representing a reduction in events of 17% (P = .04).
“We did not see a significant benefit in complete remissions after induction, but that’s not unusual,” he added. (This phenomenon of an induction randomization only having an impact upon postremission outcome, and not upon the remission rate itself, was also seen in the CCG-2891 trial, which randomized standard-timing vs intensive-timing chemotherapy, he explained.2)“We did see a reduction in the risk of relapse.”
At 3 years from the end of induction, relapses had occurred in 32.8% of the gemtuzumab ozogamicin group vs 41.3% of the standard treatment group, for a 27% reduction in risk (P = .01).
Increased Toxicity
“But we also saw an increase in treatment-related mortality,” he added. This was 6.6% in the gemtuzumab ozogamicin arm and 4.1% in the standard treatment arm among those in remission, primarily due to infections in later cycles. “Our current regimen uses four courses, not five, so we think the risk of infectious complications will be less,” he added.
“Because of this increase in toxicity, we saw no statistically significant improvement in overall survival,” he said. At 3 years from the end of induction, overall survival was 74.0% with gemtuzumab ozogamicin and 70.1% without gemtuzumab ozogamicin (P = .32).
Disease-free survival, however, closely approached a significant improvement (hazard ratio = 0.82, 95% confidence interval [CI] = 0.67–1.01, P = .07). At 3 years, disease-free survival was 60.6% vs 54.7% in the two groups, respectively.
In multivariate modeling to minimize confounding (controlling for risk group, age, white count at diagnosis, and race), the disease-free survival Cox regression hazard ratio was 0.80 (95% CI = 0.64–0.99, P = .04).
By risk subgroup, gemtuzumab ozogamicin markedly reduced relapse risk in the low-risk patient group: 19.7% with gemtuzumab ozogamicin vs 30.3% without gemtuzumab ozogamicin—a 42% reduction—but this group also had a fourfold increased risk of treatment-related mortality (7.5% vs 1.8%). Relapses were consistently reduced in all risk groups, though in the intermediate-risk and high-risk groups the benefit was limited to stem cell transplant recipients.
In conclusion, Dr. Gamis said that gemtuzumab ozogamicin and other investigational CD33-directed agents show promise in pediatric AML and merit further investigation. “We should revisit the addition of this agent, to further define the patients who would most benefit. It is very promising, and I think this is a treatment that will become more standard in the future,” he predicted. ■
Disclosure: The study authors reported no potential conflicts of interest.
References
1. Gamis AS, Aplenc R, Alonzo TA, et al: Gemtuzumab ozogamicin (GO) in children with de novo acute myeloid leukemia (AML) improves event-free survival (EFS) by reducing relapse risk: Results from the randomized phase III Children’s Oncology Group (COG) trial, AAML0531. 2013 ASH Annual Meeting. Abstract 355. Presented December 9, 2013.
2. Woods WG, Kobrinsky N, Buckley JD, et al: Timed-sequential induction therapy improves postremission outcome in acute myeloid leukemia: A report from the Children’s Cancer Group. Blood 87:4979-4989