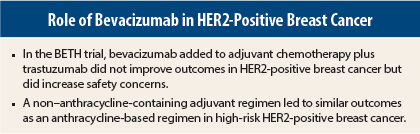
The addition of bevacizumab (Avastin) to adjuvant chemotherapy did not improve invasive disease-free survival or overall survival in patients with high-risk HER2-positive breast cancer in the large randomized phase III BETH trial. Although not specifically designed to answer this question, BETH also demonstrated that a non–anthracycline-containing chemotherapy arm was as effective in prolonging survival as an anthracycline-containing arm. The study results were presented at the 2013 San Antonio Breast Cancer Symposium.1
“In this trial, bevacizumab added virtually nothing to chemotherapy, but it did increase safety concerns. To date, all the antiangiogenic strategies studied show no impact on survival in breast cancer. Unless we can find a biomarker to identify a subgroup of patients who will benefit, bevacizumab does not warrant further study in this setting,” stated BETH study lead author Dennis Slamon, MD, PhD, Director of Clinical/Translational Research at UCLA’s Jonsson Comprehensive Cancer Center and Chief of the Division of Hematology/Oncology at UCLA.
Two-Cohort Design
The BETH trial, conducted at 576 sites around the world, enrolled 3,509 women with HER2-positive, node-positive, or high-risk node-negative breast cancer. Patients were treated in two cohorts. Cohort 1 included 3,231 patients randomly assigned to receive the nonanthracycline regimen TCH (docetaxel, carboplatin, and trastuzumab [Herceptin]) or TCH plus bevacizumab. In cohort 2, 278 patients were randomly assigned to anthracycline-based therapy with T-FEC-H (docetaxel, fluorouracil, epirubicin, cyclophosphamide, plus trastuzumab) with or without bevacizumab.
Dr. Slamon noted that anthracyclines are an established chemotherapy backbone treatment in breast cancer, including HER2-positive breast cancer. However, the combination of trastuzumab plus anthracycline increases the risk of cardiotoxicity—in particular, congestive heart failure—and secondary leukemia.
About 130 centers had the option to select an anthracycline-based regimen. Dr. Slamon noted that he was disappointed that fewer than 300 patients were assigned to anthracyclines, resulting in less power to compare the anthracycline vs nonanthracycline regimen. Treatment arms were well balanced for age, number of positive lymph nodes, breast-conserving surgery, and hormone receptor status. Median age was 51 years.
Key Data
At a median follow-up of 38 months, the rate of invasive disease–free survival in cohort 1 was 92% in both TCH arms (with and without bevacizumab), and in cohort 2, 89% in the anthracycline-containing arms without bevacizumab vs 91% with bevacizumab. This difference between the anthracycline and non–anthracycline-containing arms was not statistically significant.
Dr. Slamon pointed out that the 92% invasive disease–free survival achieved in both TCH treatment arms surpassed results of other large randomized trials in HER2-positive breast cancer. For example, 3-year disease-free survival was about 87% in both the Herceptin Adjuvant (HERA) trial2 and the N9831 trial.3 He noted that the negative showing for adjuvant bevacizumab in BETH might be partly attributable to the excellent 92% disease-free survival in the TCH control arm.
“It is going to be difficult to develop treatment regimens that have even better response rates than that. While there is some small room for improvement, we now need to concentrate further on improving the safety of adjuvant treatment regimens,” Dr. Slamon commented.
Safety Concerns
No new safety concerns about bevacizumab were raised in BETH, but bevacizumab significantly increased the risk of any-grade and grade 3/4 adverse events, as well as adverse events of special interest such as hypertension and proteinuria (all P < .0001).
Patients enrolled in BETH will be followed prospectively to determine longer-term outcomes. Dr. Slamon said he believes that the TCH regimen is driving the disease-free survival benefit, and he doubted whether bevacizumab would make a significant difference over the longer term.
Experts—including Dr. Slamon—pretty much agree that bevacizumab has no role in adjuvant therapy of breast cancer.
“Although the data are somewhat mixed, with one previous trial in metastatic disease and a recent neoadjuvant trial showing a slight advantage for bevacizumab, the cumulative data including the BETH adjuvant trial suggest minimal if any value for this drug in breast cancer,” said C. Kent Osborne, MD, Director of the Dan L. Duncan Cancer Center and the Lester and Sue Smith Breast Center at Baylor College of Medicine, Houston.
Anthracycline vs Nonanthracycline
Use of an anthracycline in early breast cancer is controversial, and experts are basically divided into camps on this issue.
“Trastuzumab combined with anthracyclines increases cardiac toxicity three- to fivefold,” Dr. Slamon explained. “Our new results, which surpassed our expectations, show that it is not necessary to include an anthracycline as part of the treatment regimen to obtain ideal results for patients with HER2-positive breast cancer, even if they have a large tumor or node-positive disease,” Dr. Slamon told listeners at a press conference during the San Antonio meeting. “The importance of these results lies in the fact that TCH has a much better safety profile than anthracycline/trastuzumab combinations and has now been shown to be equally
effective.”
He continued, “No single trial has shown an incremental benefit for anthracyclines…. At our institution, we don’t use anthracyclines as adjuvant therapy for early HER2-positive breast cancer.”
Press conference moderator Jennifer Litton, MD, a breast medical oncologist at The University of Texas MD Anderson Cancer Center, Houston, expressed a different opinion. “We could debate this for 5 hours. I am on the other side of the aisle on this question, and I don’t think anthracyclines should be thrown away.” She pointed out that the BETH trial was designed to evaluate the role of bevacizumab in early HER2-positive breast cancer, not to show a difference between anthracyclines vs no anthracyclines. ■
Disclosure: The BETH study was supported by Roche/Genentech. Dr. Slamon is a consultant for and receives research support from Novartis, and has ownership interests in Amgen.
References
1. Slamon DL, Swain SM, Buyse M, et al: Primary results from BETH, a phase 3 controlled study of adjuvant chemotherapy and trastuzumab ± bevacizumab in patients with HER2-positive, node-positive, or high-risk node-negative breast cancer. 2013 San Antonio Breast Cancer Symposium. Abstract S1-03. Presented December 11, 2014.
2. Goldhirsch A, Geler RD, Piccart-Gebhart M, et al: 2 years versus 1 year of adjuvant trastuzumab for HER2-positive breast cancer (HERA): An open-label, randomized controlled trial. Lancet 382:1021-1028, 2013.
3. Romond EH, Perez EA, Bryant J, et al: Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med 353:1673-1684, 2005.