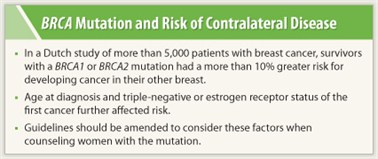
Patient and tumor characteristics can stratify women with breast cancer and a BRCA mutation into groups having different risks of contralateral disease, which may help tailor follow-up, suggests a study of more than 5,000 women in the Netherlands. Confirming findings of other studies, the study found that the cumulative 10-year risk of developing cancer in the other breast was significantly higher for BRCA mutation carriers than for noncarriers, according to results reported at the 2011 San Antonio Breast Cancer Symposium.1 However, age and tumor receptor status had modifying effects, enabling splitting of the carriers into subgroups having very different risks.
Study Background
 “Studies show that certain subgroups of women [with a BRCA mutation] who have already had cancers are also at risk for developing a second new cancer in their other breast, much more so than survivors who do not carry the mutation,” said Alexandra J. van den Broek, MSc, a doctoral candidate at the Netherlands Cancer Institute. “Our study is, as far as we know, the first study showing that within certain carriers of BRCA mutations, subgroups with an increased or decreased risk for contralateral breast cancer can be made.”
“Studies show that certain subgroups of women [with a BRCA mutation] who have already had cancers are also at risk for developing a second new cancer in their other breast, much more so than survivors who do not carry the mutation,” said Alexandra J. van den Broek, MSc, a doctoral candidate at the Netherlands Cancer Institute. “Our study is, as far as we know, the first study showing that within certain carriers of BRCA mutations, subgroups with an increased or decreased risk for contralateral breast cancer can be made.”
Researchers surveyed 5,061 women diagnosed with unilateral, invasive breast cancer at 10 hospitals in the Netherlands. A total of 211 women (4.2%) were carriers of the BRCA1 or BRCA2 mutation. Overall, at a median of 8.4 years of follow-up, 8.6% of participants developed contralateral breast cancer. Ms. Van den Broek and colleagues found that the overall 10-year risk for developing contralateral breast cancer in noncarriers was 6.0%, whereas risk for carriers was 17.9%.
For carriers diagnosed with their first breast cancer when younger than 40 years, the 10-year risk for contralateral breast cancer jumped to 26.0%. For carriers between the ages of 40 and 50 years at first diagnosis, the risk was 11.6%. In addition, mutation carriers with a triple-negative first tumor had a 10-year cumulative contralateral breast cancer risk of 18.9%, compared with 11.2% among carriers with a non–triple-negative first tumor.
Important for Counseling
Although these numbers can be overwhelming to carriers who have already survived breast cancer, Ms. van den Broek said it is crucial to know who is most at risk and by how much.
“Guidelines for prophylactic measures and screening in the follow-up of patients with breast cancer carrying the BRCA1 or BRCA2 mutation are important to provide patients with the best information and counseling,” she said. “If these results are confirmed, [it will be] possible to personalize the guidelines for these specific subgroups.”
The next step will be to confirm the results in larger studies and to look at other factors that define subgroups of patients with an increased or decreased risk for CBC.
Clinically Useful Information
 This is “really clinically useful information,” commented Laura J. Esserman, MD, of the UCSF Helen Diller Family Comprehensive Cancer Center during the question-and-answer period.
This is “really clinically useful information,” commented Laura J. Esserman, MD, of the UCSF Helen Diller Family Comprehensive Cancer Center during the question-and-answer period.
“Modeling studies have suggested that BRCA2 carriers, particularly at older ages, don’t benefit very much, certainly not much in terms of survival, from prophylactic mastectomy,” Dr. Esserman noted. Given the study’s results for women aged 40 to 50, “I think this would support that the benefit of prophylactic mastectomy would be quite small” in older BRCA2 mutation carriers. ■
Disclosure: Ms. van den Broek and Dr. Esserman reported no potential conflicts of interest.
Reference
1. van den Broek AJ, Schmidt MK, Tollenaar RAEM, et al: The risk of contralateral breast cancer in BRCA1/2 carriers compared to non-BRCA1/2 carriers in an unselected cohort. San Antonio Breast Cancer Symposium. Abstract S4-2. Presented December 8, 2011.

