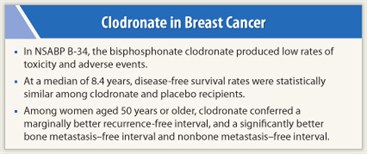
A benefit of the oral bisphosphonate clodronate when used as adjuvant therapy for early breast cancer may depend on factors such as the endpoint assessed and patient age, suggests the randomized B-34 trial conducted by the National Surgical Adjuvant Breast and Bowel Project (NSABP).
The trial, conducted among 3,323 women, failed to meet its primary endpoint, finding no significant gain in disease-free survival with clodronate vs placebo, investigators reported at the San Antonio Breast Cancer Symposium.1 But in the subset of women aged 50 years or older, there were 26% to 39% reductions in the risks of recurrence and metastases with clodronate.
Vicious Cycle?
 These findings add to accumulating evidence that suggests it may be time to modify the vicious-cycle hypothesis of bone metastases, whereby cancer cells and bone cells mutually drive each other in promoting bone resorption, according to lead investigator Alexander H.G. Paterson, MD, who is an investigator with the NSABP in Pittsburgh and a Professor at the University of Calgary in Canada.
These findings add to accumulating evidence that suggests it may be time to modify the vicious-cycle hypothesis of bone metastases, whereby cancer cells and bone cells mutually drive each other in promoting bone resorption, according to lead investigator Alexander H.G. Paterson, MD, who is an investigator with the NSABP in Pittsburgh and a Professor at the University of Calgary in Canada.
In “the new vicious cycle, cancer accelerates osteoclast function and bone destruction—I think we agree on [that],” he said. “However, inhibition of osteoclast function with bisphosphonates has an effect on cancer growth in older women but little effect in premenopausal women.”
Disparities between Trials
The overall B-34 findings differ from those of another adjuvant clodronate trial, which found a reduced risk of bone metastases.2 The disparity is likely due to differences in endpoints and patients, speculated Dr. Paterson.
 Several components of disease-free survival—contralateral breast cancers, second primaries, and death from any cause—“may not have a direct relevance for an agent that has its prime effect on bone,” he explained. Additionally, the B-34 patients had “earlier breast cancer and lower rates of events, and the majority were over the age of 50.”
Several components of disease-free survival—contralateral breast cancers, second primaries, and death from any cause—“may not have a direct relevance for an agent that has its prime effect on bone,” he explained. Additionally, the B-34 patients had “earlier breast cancer and lower rates of events, and the majority were over the age of 50.”
“I’ve stated my concerns all the way through this trial” regarding the choice of primary endpoint and its possible weakening of the ability to assess secondary endpoints, concurred Trevor J. Powles, PhD, of the Royal Marsden Hospital, London, who was lead investigator on the earlier clodronate trial. “Clodronate may be different from zoledronate because we are looking at an agent [for which] we really have no evidence that it does anything but work on bone.”
Clinical Impact
 Session moderator Julie R. Gralow, MD, Director of Breast Oncology at the University of Washington, Seattle, questioned what the new B-34 findings mean for clinical care. “Clodronate is approved in Canada, but it’s not approved in the U.S. Are you going to start using it when you go home?” she asked Dr. Paterson.
Session moderator Julie R. Gralow, MD, Director of Breast Oncology at the University of Washington, Seattle, questioned what the new B-34 findings mean for clinical care. “Clodronate is approved in Canada, but it’s not approved in the U.S. Are you going to start using it when you go home?” she asked Dr. Paterson.
“I think we have to start thinking about this,” he replied. “It’s an easy treatment, it’s oral, it seems to have an effect in older women and at low toxicity. We’ve now got four trials showing the same direction. There are differences in the patients, and you are going to get differences in the statistics. But they are all pointing in the same direction—that is, benefit in older patients.”
In an interview, Dr. Gralow further noted that data from bisphosphonate trials are gradually sorting out a possible role for these agents in adjuvant therapy, which may ultimately lead to less intensive treatment for some patients. There is “clearly something going on with age, estrogen status, and bone resorption,” she agreed.
Additionally, trials such as AZURE3 suggest that bisphosphonates may have less benefit in patients given chemotherapy, possibly because that therapy already prevents many recurrences. “We have to figure out the population [who benefit],” Dr. Gralow commented. “I’d like to back off on giving chemo … if we can figure out who the bisphosphonates really work in—is it a group that doesn’t get chemo? A group that is postmenopausal or has a high bone resorption state?”
Study Details
 In the B-34 trial, women with early breast cancer, regardless of receipt of chemotherapy and/or tamoxifen, were assigned in balanced fashion to 3 years of treatment with clodronate or placebo. They predominantly were aged 50 years or older (64%), had node-negative disease (75%), and had tumors with hormone receptors (78%).
In the B-34 trial, women with early breast cancer, regardless of receipt of chemotherapy and/or tamoxifen, were assigned in balanced fashion to 3 years of treatment with clodronate or placebo. They predominantly were aged 50 years or older (64%), had node-negative disease (75%), and had tumors with hormone receptors (78%).
The time on assigned treatment was significantly shorter in the clodronate group than in the placebo group. Overall, 40% of patients did not complete 3 years of treatment.
“The drop in compliance really occurred in the first 6 months, when patients were also receiving intravenous chemotherapy,” Dr. Paterson noted. “Compliance might have been better if we had started a little later.”
The incidence of grade 3 or higher toxicity was similar with clodronate and placebo (20% and 22%). There was a single case of possible osteonecrosis of the jaw with clodronate.
Key Findings
With a median follow-up of 8.4 years, the rate of disease-free survival was statistically indistinguishable between groups. Overall, 17.3% of women in the clodronate group and 18.8% of women in the placebo group had an event.
In terms of secondary endpoints, the clodronate group had a significantly longer nonbone metastasis–free interval (HR = 0.74), Dr. Paterson reported.
Analyses among predefined subgroups showed no significant improvement in disease-free survival with clodronate. But among women aged 50 years or older at diagnosis, the drug conferred a marginally better recurrence-free interval (HR = 0.76) and a significantly better bone metastasis–free interval (HR = 0.61) and nonbone metastasis–free interval (HR = 0.63).
In post hoc analyses, relative reductions in risks of skeletal metastases and nonskeletal metastases with clodronate increased in “stepwise” fashion with age, further pointing to a role for the “estrogen micromilieu,” according to Dr. Paterson. ■
Disclosure: Dr. Gralow receives research support from Amgen, Novartis, and Roche. Dr. Paterson has been a consultant for Amgen and receives clinical trials funding from Amgen. Dr. Powles reported no potential conflicts of interest.
References
1. Paterson AHG, Anderson SJ, Lembersky BC, et al: NSABP protocol B-34: A clinical trial comparing adjuvant clodronate vs. placebo in early stage breast cancer patients receiving systemic chemotherapy and/ortamoxifen or no therapy—final analysis. San Antonio Breast Cancer Symposium. Abstract S2-3. Presented December 7, 2011.
2. Powles T, Paterson A, McCloskey E, et al: Reduction in bone relapse and improved survival with oral clodronate for adjuvant treatment of operable breast cancer [ISRCTN83688026]. Breast Cancer Res 8(2):R13, 2006.
3. Coleman RE, Marshall H, Cameron D, et al: AZURE Investigators. Breast-cancer adjuvant therapy with zoledronic acid. N Engl J Med 365:1396-1405, 2011.

