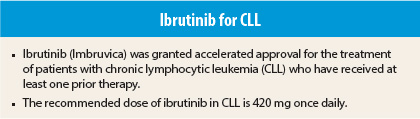
On February 12, 2014, ibrutinib (Imbruvica) was granted accelerated approval for the treatment of patients with chronic lymphocytic leukemia (CLL) who have received at least one prior therapy.1,2 Ibrutinib previously received accelerated approval for the treatment of patients with mantle cell lymphoma who have received at least one prior therapy.
Efficacy Findings
The approval in CLL is based on results of a multicenter, single-arm trial of 48 patients with previously treated CLL. Patients had a median age of 67 years (range, 37–82 years; 52% ≥ 65 years), 71% were male, all had Eastern Cooperative Oncology Group performance status of 0 or 1, median time from diagnosis was 6.7 years, and median number of prior treatments was four (range, 1–12).
Ibrutinib was given orally at 420 mg once daily until disease progression or unacceptable toxicity. Ibrutinib treatment produced a 58.3% overall response rate (95% confidence interval = 43.2%–72.4%) on independent review committee assessment. No complete responses were observed. Response duration ranged from 5.6 to more than 24.2 months, with median response not being reached. No overall differences in effectiveness were observed between patients aged ≥ 65 years and younger patients.
As a condition of accelerated approval in CLL, the U.S. Food and Drug Administration (FDA) requires that the sponsor submit results of a randomized clinical trial. In January 2014, Pharmacyclics notified FDA that the phase III RESONATE trial comparing ibrutinib vs ofatumumab (Arzerra) in patients with previously treated CLL or small lymphocytic lymphoma who were not candidates for purine analog–based treatments had been stopped early on the basis of favorable results in a planned interim analysis. The trial was reported to demonstrate improvement in progression-free survival and overall survival with ibrutinib.
How It Works
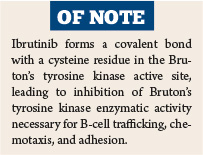
Ibrutinib is a small-molecule inhibitor of Bruton’s tyrosine kinase, a signaling molecule of the B-cell antigen receptor and cytokine receptor pathways. Bruton’s tyrosine kinase activity in signaling through the B-cell surface receptor results in activation of pathways necessary for B-cell trafficking, chemotaxis, and adhesion.
Ibrutinib forms a covalent bond with a cysteine residue in the Bruton’s tyrosine kinase active site, leading to inhibition of Bruton’s tyrosine kinase enzymatic activity. Preclinical studies have shown that ibrutinib inhibits malignant B-cell proliferation and survival in vivo and cell migration and substrate adhesion in vitro.
How It Is Given
The recommended dose of ibrutinib in CLL is 420 mg once daily. Ibrutinib treatment should be interrupted for grade 3 or higher nonhematologic toxicities, grade 3 or higher neutropenia with fever, and grade 4 hematologic toxicities. With resolution to grade 1 or baseline status, treatment can be reinitiated at the starting dose. The dose may be reduced to 280 mg and then to 140 mg for recurrent toxicity.
Coadministration of ibrutinib with strong or moderate CYP3A inhibitors (eg, clarithromycin, grapefruit juice, indinavir, ketoconazole) should be avoided. If a strong inhibitor is to be used for ≤ 7 days, interruption of ibrutinib during this period can be considered. If a moderate inhibitor must be used, the ibrutinib dose should be reduced to 140 mg. Patients taking concomitant strong or moderate CYP3A inhibitors should be monitored more closely for signs of ibrutinib toxicity.
Ibrutinib exposure is not altered in patients with creatinine clearance > 25 mL/min; there are no data in patients with severe renal impairment or on dialysis. Since ibrutinib is metabolized in the liver, significant increases in exposure are expected in patients with hepatic impairment and patients with serum aspartate transaminase or alanine transaminase at least 3.0 times the upper limit of normal were excluded from clinical trials. Data are insufficient to recommend a dose in patients with hepatic impairment.
Safety Profile
The most common adverse events of any grade in the CLL trial were thrombocytopenia (71%), diarrhea (63%), bruising (54%), neutropenia (54%), upper respiratory tract infection (48%), anemia (44%), and fatigue (31%). The most common grade 3 or 4 adverse events were neutropenia (27%), thrombocytopenia (10%), pneumonia (8%), and hypertension (8%).
Patients aged ≥ 65 years had a higher frequency of adverse events, including grade 3 or higher adverse events (80% vs 61%). Second malignancies occurred in 10% of patients, with one patient dying from histiocytic sarcoma. Adverse events resulted in treatment discontinuation in 10% of patients (6% due to infection and 4% due to subdural hematoma) and in dose reduction in 13%. Shifts from normal to elevated uric acid levels occurred in 38% of patients, including 4% with levels >10 mg/dL.
Ibrutinib carries warnings/precautions for hemorrhage, infections, myelosuppression, renal toxicity, second primary malignancies (including skin cancers and other carcinomas), and embryo-fetal toxicity. Patients must be monitored for bleeding and for fever and infections. Renal function must be monitored and adequate hydration ensured. Complete blood counts should be monitored monthly. Women must be advised of potential fetal risk and counseled to avoid pregnancy while taking ibrutinib. ■
In the Clinic provides overviews of novel oncology agents, addressing indications, mechanisms, administration recommendations, safety profiles, and other essential information needed for the appropriate clinical use of these drugs.
References
1. U.S. Food and Drug Administration: Ibrutinib (IMBRUVICA). Available at www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm385878.htm.
2. IMBRUVICATM (ibrutinib) capsules prescribing information. Pharmacyclics, Inc, February, 2014. Available at www.accessdata.fda.gov/drugsatfda_docs/label/2014/203147s000lbl.pdf.