Anti–PD-1 antibodies have been shown to be effective in solid tumors. There is evidence that the malignant Reed-Sternberg cells in Hodgkin lymphomas use the programmed cell death protein 1 (PD-1) pathway to evade immune detection, with alterations in chromosome 9p24.1 increasing levels of the PD-1 ligands PD-L1 and PD-L2 through JAK-STAT signaling. In an ongoing phase I study reported in The New England Journal of Medicine, Stephen M. Ansell, MD, PhD, of Mayo Clinic, and colleagues found that treatment with the PD-1 inhibitor nivolumab (Opdivo) produced a high response rate in heavily pretreated patients with Hodgkin lymphoma.1
Study Details
In the study, 23 patients with relapsed/refractory Hodgkin lymphoma received nivolumab at 3 mg/kg every 2 weeks until complete response, disease progression, or excessive toxicity. Patients had a median age of 35 years (range, 20–54 years); 12 (52%) were male; 20 (87%) were white; Eastern Cooperative Oncology Group performance status was 0 in 6 (26%) and 1 in 17 (74%); 22 (96%) had nodular sclerosis; number of previous systemic therapies was 2 or 3 in 8 (35%), 4 or 5 in 7 (30%), and ≥ 6 in 8 (35%); 4 (17%) had extranodal involvement; 19 (83%) had previous radiotherapy; and 18 (73%) enrolled in the study after relapse following autologous stem cell transplantation and 18 (73%) after relapse following brentuximab vedotin (Adcetris) treatment.
Responses
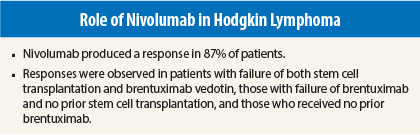
An objective response occurred in 20 patients (87%), including 4 (17%) with a complete response and 16 (70%) with a partial response; the remaining 3 patients (13%) had stable disease. Of the 4 patients with a complete response, 3 had not received previous brentuximab vedotin.
Among 15 patients with tumor recurrence after autologous stem cell transplantation and brentuximab vedotin, the response rate was 87%, with 1 patient (7%) having a complete response, 12 (80%) a partial response, and 2 (13%) stable disease. All 3 patients who did not undergo autologous stem cell transplantation before brentuximab vedotin treatment had partial responses.
Among 5 patients who did not receive brentuximab vedotin, 4 (80%) had responses, including complete response in 3, and 1 patient had stable disease. In the 20 patients who responded, 12 (60%) had the first response by 8 weeks (range, 3–39 weeks).
Additional Results
Progression-free survival at 24 weeks was 86% (95% confidence interval = 62%–95%). At the time of reporting, 6 patients had chosen to undergo stem cell transplantation at the time of the best overall response, and 11 patients continued to maintain response. Median overall survival had not been reached after median duration of follow-up of 40 weeks (range, 0–75 weeks).
Analyses of pretreatment tumor specimens from 10 patients showed PDL1 and PDL2 copy number increases and increased expression of the ligands. Reed-Sternberg cells showed nuclear positivity of phosphorylated STAT3, indicating active JAK-STAT signaling.
Treatment Exposure and Adverse Events
Patients received a median of 16 nivolumab doses (range, 6–37) over a median treatment duration of 36 weeks (range, 13–77), with 15 patients (65%) receiving ≥ 90% of the intended overall dose. Reasons for discontinuation of treatment included stem cell transplantation in 6 patients, disease progression in 4 patients, and drug toxicity in 2 patients.
The most common drug-related adverse events of any grade were rash (22%), decreased platelets (17%), fatigue (13%), pyrexia (13%), diarrhea (13%), nausea (13%), and pruritus (13%). No drug-related grade 4 or 5 adverse events were reported. Drug-related grade 3 adverse events occurred in 5 patients (22%) and included myelodysplastic syndrome, pancreatitis, pneumonitis, stomatitis, colitis, gastrointestinal inflammation, thrombocytopenia, increased lipase level, decreased lymphocyte level, and leukopenia.
Serious adverse events occurred in 3 patients, consisting of grade 3 pancreatitis, grade 3 myelodysplastic syndrome, and grade 2 lymph node pain. The patient with myelodysplastic syndrome had undergone six previous systemic chemotherapies, radiation therapy, and autologous stem cell transplantation but had not received prior bendamustine (Treanda).
Dose delay was required in 9 patients (39%) and was due to nonhematologic adverse events in 5. The adverse events leading to treatment discontinuation were myelodysplastic syndrome and thrombocytopenia in 1 patient and pancreatitis in 1 patient. Infusion was interrupted in 2 patients (9%) due to grade 1 hypersensitivity reaction.
The investigators concluded:
“Nivolumab had substantial therapeutic activity and an acceptable safety profile in patients with previously heavily treated relapsed or refractory Hodgkin’s lymphoma.” They noted: “The frequent clinical responses to nivolumab therapy in heavily pretreated patients with relapsed or refractory Hodgkin’s lymphoma and genetic alterations of the PD-1 ligand loci highlight the importance of the PD-1 immune evasion pathway and the genetically defined sensitivity to PD-1 blockade in this disease.”
Dr. Ansell, Alexander M. Lesokhin, MD, of Memorial Sloan Kettering Cancer Center, Margaret A. Shipp, MD, of Dana-Farber Cancer Institute, and Philippe Armand, MD, PhD, of Dana-Farber Cancer Institute, contributed equally to The New England Journal of Medicine article. ■
Disclosure: The study was funded by Bristol-Myers Squibb and others. For full disclosures of the study authors, visit www.nejm.org.
Reference
1. Ansell SM, Lesokhin AM, Borrello I, et al: PD-1 blockade with nivolumab in relapsed or refractory Hodgkin’s lymphoma. N Engl J Med 372:311-319, 2015.