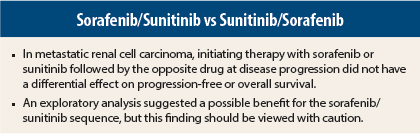
The explosion of new therapies for metastatic renal cell carcinoma is a welcome advance, but studies have not yet defined optimal sequencing of the newer therapies. According to the phase III SWITCH trial, it matters little whether therapy for metastatic renal cell carcinoma begins with sorafenib (Nexavar) and is followed by sunitinib (Sutent) or vice versa. Both sequences achieved comparable progression-free and overall survival, and safety was consistent with previous reports on both drugs. Results of the study were presented at the Genitourinary Cancers Symposium in San Francisco.1
“This is the first randomized, prospective study of first-line sequential therapy with [sorafenib/sunitinib] vs [sunitinib/sorafenib] for advanced or metastatic renal cell carcinoma. The primary objective of this trial was not met because neither sequence achieved superior total progression-free survival. Overall survival was similar in both arms. Safety profiles were as expected,” said lead author Maurice Stephan
Michel, MD, PhD, Medical Director of the Department of Urology at University Hospital Mannheim, Germany.
SWITCH Trial Details
SWITCH was a prospective, open-label, randomized, phase III trial conducted in Germany, Austria, and the Netherlands. Patients (N = 365) with advanced or metastatic renal cell carcinoma who were not suitable candidates for cytokine therapy and had not received prior systemic therapy for advanced disease were randomly assigned 1:1 to first-line therapy with sorafenib or sunitinib; at the time of disease progression or intolerable toxicity, they were transitioned to second-line therapy with sunitinib or sorafenib, respectively. The primary endpoint was total progression-free survival, defined as the time from randomization to confirmed progression or death during second-line therapy.
At baseline, demographic and disease characteristics were similar for the two treatment arms. Median age was around 64 years, about 75% were male, and about 86% had clear-cell histology. Most patients were classified as intermediate-risk according to Memorial Sloan Kettering Cancer Center criteria, but the sunitinib/sorafenib arm had slightly more favorable-risk patients (39% in the sorafenib/sunitinib arm and 44.8% in the sunitinib/sorafenib arm).
At the end of the study, 11% of the sunitinib/sorafenib group were still on first-line sunitinib and 9% of the sorafenib/sunitinib group were still on first-line sorafenib. Second-line therapy was delivered to 42% of sunitinib/sorafenib recipients and 57% of sorafenib/sunitinib recipients. By study’s end, 3% and 7%, respectively, were still on second-line therapy.
Key Results
No significant difference was observed between the two treatment arms for the primary endpoint of total progression-free survival. Median total progression-free survival was 12.5 months for sorafenib/sunitinib vs 14.9 months for sunitinib/sorafenib (hazard ratio [HR] = 1.01, P = .54).
Overall survival was also not significantly different between the two arms. Median overall survival was 31.5 months for sorafenib/sunitinib vs 30.2 months for sunitinib/sorafenib (HR = 0.997, P = .49).
Dr. Michel said it would be difficult with current therapies to beat overall survival of more than 30 months. “This is among the longest survival reported in metastatic renal cell carcinoma,” he stated.
An analysis evaluating second-line therapy found a significant difference in disease control rate favoring the sorafenib/sunitinib arm: 48.5% vs 31.6%, respectively (P = .03). However, these results may be biased, Dr. Michel pointed out, as more patients were able to get second-line therapy in the sorafenib/sunitinib arm (56.6% vs 41.5%, respectively; P < .01).
Adverse Effects
Side effects after first-line therapy were as expected and differed by drug. Treatment-emergent diarrhea and skin reactions were more common when sorafenib was used as first-line therapy, whereas nausea and stomatitis were more common with first-line sunitinib.
Adverse events were generally less frequent during second-line therapy than first-line therapy, which may reflect “survival of the fittest” to reach second-line therapy. Neither drug had any effect on cardiac safety. ■
Disclosure: SWITCH was sponsored by the German Cancer Society with a financial grant from Bayer Pharma AG, marketers of sorafenib. Dr. Michel has received honoraria from Astellas Pharma, Bayer, and Novartis. For full disclosures of the study authors, visit abstracts.asco.org.
Reference
1. Michel MS, Vervenne W, de Santis M, et al: SWITCH: A randomized sequential open-label study to evaluate efficacy and safety of sorafenib/sunitinib versus sunitinib/sorafenib in the treatment of metastatic renal cell carcinoma. 2014 Genitourinary Cancers Symposium. Abstract 393. February 1, 2014.