
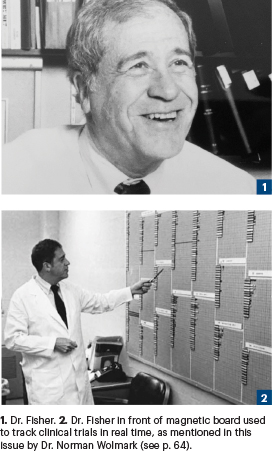
Photo: NCI
Bernard Fisher, MD, who died on October 16, 2019, at the age of 101, is recognized today for his groundbreaking research in breast cancer, which ultimately ended the standard practice of performing the Halsted radical mastectomy, a treatment that had been in place for more than 75 years. His laboratory and clinical investigations led to more effective therapy, increased survival rates, and improved quality of life for women with breast cancer.
His early medical career, however, was focused primarily on liver regeneration and transplantation.
Born in Pittsburgh on August 23, 1918, Dr. Fisher’s early school career was marked by a love and talent for science. He graduated from Taylor Allderdice High School in 1936 and attended the University of Pittsburgh Medical School. After graduating from the University of Pittsburgh School of Medicine in 1943 and completing a 2-year fellowship in experimental surgery at the University of Pennsylvania, Dr. Fisher returned to the University of Pittsburgh to create a surgical research laboratory, where he began experiments on rats to determine whether their livers would regenerate after large portions were removed. Finding they did, he began transplanting various organs in rats. In 1955, to increase his knowledge about transplantation, Dr. Fisher served as a research fellow at the London Postgraduate Medical School, Hammersmith Hospital.
Novel Approaches to Treatment
When he returned to Pittsburgh the following year, Dr. Fisher received a call from I.S. Ravdin, MD, his mentor at the University of Pennsylvania. That call would permanently alter the course of his scientific and clinical career. Dr. Ravdin, then Chairman of the Clinical Studies Panel of the Cancer Chemotherapy National Service Center at the National Institutes of Health (NIH), asked Dr. Fisher to attend a meeting with 22 other surgeons to discuss the creation of the Surgical Adjuvant Chemotherapy Breast Project, which later became known as the National Surgical Adjuvant Breast and Bowel Project -(NSABP), chaired by Dr. Fisher for 30 years.
Although Dr. Fisher was initially hesitant to change the focus of his research from liver regeneration and transplantation to breast cancer and the study of malignant disease, he was intrigued by the question of how tumors metastasize.
“I do believe my greatest contribution was carrying out laboratory investigations, beginning in 1950, which have altered our understanding and treatment of breast cancer.”— Bernard Fisher, MD
Tweet this quote
The meeting at the NIH resulted in the 1958 launch of the first randomized clinical trial to evaluate the use of systemic therapy following radical mastectomy in the treatment of breast cancer.1,2 More than 800 women treated with the surgery were enrolled in the study and randomly assigned to receive either the alkylating agent thiotepa or a placebo. The study found that although the drug provided a significant benefit in recurrence-free survival in premenopausal women, altering the course of their breast cancer, the fact that chemotherapy did not benefit all patients and caused some side effects made physicians reluctant to embrace the use of systemic adjuvant therapy.
In a past interview with The ASCO Post, Dr. Fisher said: “Subsequent to that first meeting at the NIH, I discovered how little information there was related to the biology of breast cancer and what a lack of interest there was in understanding the disease. At the meeting, I learned about the need for randomized clinical trials and the use of biostatistics to obtain credible information from those trials.”
Biology of Tumor Metastasis
After that meeting, Dr. Fisher abandoned his research in liver regeneration and transplantation and devoted the next 4 decades to pursuing the biology of breast cancer tumor metastasis and more effective treatments for the disease. His research led him away from the anatomic hypothesis presented by Halsted—that cancer cells, originating from the breast, always passed through the lymph nodes prior to metastatic spread and, therefore, required radical surgery to remove the entire breast, underlying chest muscle, and axillary lymph nodes to halt metastasis.
Instead, Dr. Fisher proposed, breast cancer is a systemic disease in which malignant cells are likely disseminated throughout the body before diagnosis, and radical mastectomies are unlikely to improve overall survival. Breast-sparing surgery such as lumpectomy, in which only the cancerous tumor and a small portion of the surrounding tissue are removed, would probably result in similar outcomes but without the disfigurement caused by total mastectomy, reasoned Dr. Fisher.
Throughout the 1960s and 1970s, Dr. Fisher conducted laboratory investigations of cancer biology and randomized clinical studies evaluating the effectiveness of lumpectomy vs total mastectomy, as well as lumpectomy followed by systemic chemotherapy or radiation therapy in the prevention of disease recurrence. The use of less aggressive, breast-conserving surgical treatment was initially met with resistance from both the medical establishment and the general public—resistance he looked back on as “extensive and often unpleasant.” Dr. Fisher’s findings, however, indicated breast cancer metastasis is not solely determined by anatomic considerations, but is also influenced by the biologic activity of both the tumor and the host.
“The results obtained from those studies led me to form a biologic hypothesis that replaced the Halstedian principles, which governed the treatment of breast cancer for almost a century.”— Bernard Fisher, MD
Tweet this quote
The results from those early studies changed the way breast cancer is treated and are credited with improving breast cancer survival rates. In 1991, Dr. Fisher and his NSABP colleagues began the first breast cancer prevention trial, which tested the efficacy of tamoxifen in preventing breast cancer in high-risk women. The study found that tamoxifen did decrease the incidence of both invasive and noninvasive breast cancers by nearly 50%.3
Six-Decade Legacy
Dr. Fisher served as ASCO President from 1992 to 1993 and has received numerous awards for his contributions to breast cancer research and treatment, including the American Association for Cancer Research Award for Lifetime Achievement in Cancer Research, the American Cancer Society Medal of Honor, and the Albert Lasker Clinical Medical Research Award.
When asked in an earlier interview what he considered his greatest contributions to medicine and science, Dr. Fisher replied: “That question might be best answered by others who are familiar with my efforts over the past 60 years. However, I do believe my greatest contribution was carrying out laboratory investigations, beginning in 1950, which have altered our understanding and treatment of breast cancer. The results obtained from those studies led me to form a biologic hypothesis that replaced the Halstedian principles, which governed the treatment of breast cancer for almost a century.”
REFERENCES
1. NSABP Timeline. Available at nsabp.pitt.edu/NSABP Timeline.pdf. Accessed May 12, 2020.
2. Fisher B, Ravdin RG, Ausman RK, et al: Surgical adjuvant chemotherapy in cancer of the breast: Results of a decade of cooperative investigation. Ann Surg 168:337-356, 1968.
3. Fisher B, Costantino JP, Wickerham DL, et al: Tamoxifen for prevention of breast cancer: Report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst 90:1371-1388, 1998.


